Natural Shoulder Pain Relief
The shoulder joint or (glenohumeral joint) is a ball and socket joint enabling ample movement. Because it is one of the most mobile joints in the human body, joint stability is sacrificed predisposing it to injury.
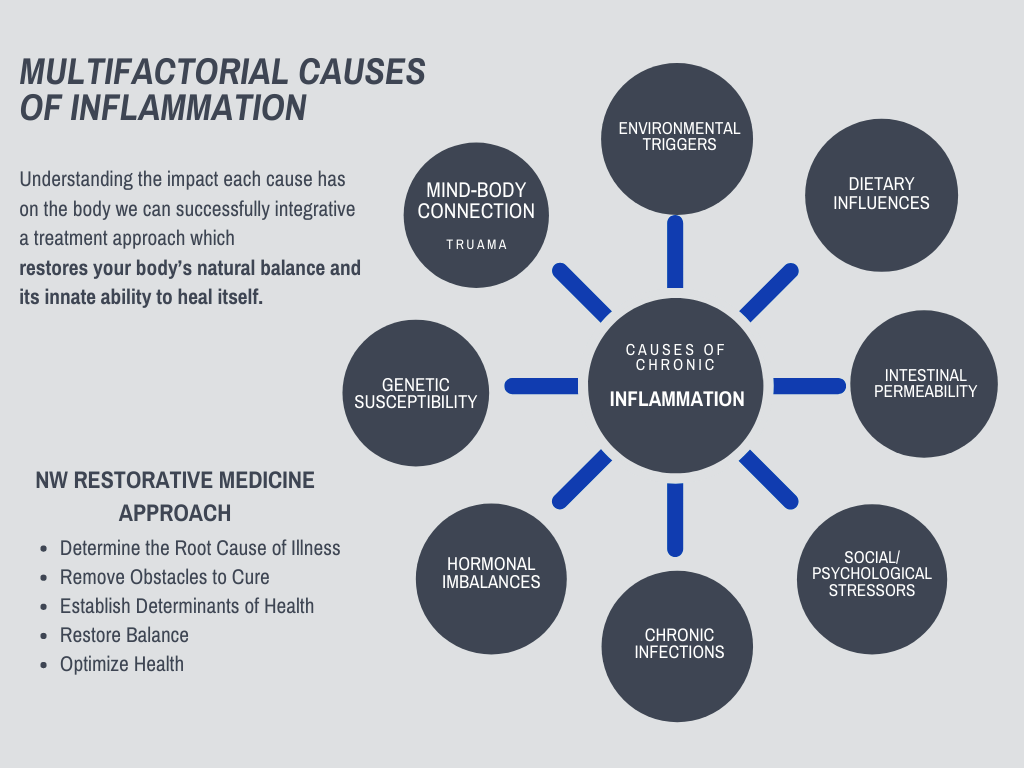
Your Shoulder is Connected to Your Whole Body, and so is Your Pain and Inflammation
As a result, the cause of shoulder pain and inflammation comes from many factors, requiring a whole-body approach to relieving pain.
Dr. Squires’ approach brings together a holistic treatment of all the factors contributing to your chronic inflammation and pain. Personalizing treatment to the factors most impacting your source of pain.
And combines it with a Regenerative Medicine approach that stimulates your own body’s healing response naturally.
Regenerative medicine is a cell-based therapy using advanced scientific techniques in the treatment of degenerative disease, orthopedic injuries, and joint conditions.
Discover how Dr. Squires can help by scheduling an initial consult »
Common Shoulder Injuries Treated:
Rotator Cuff Tendinopathy and/or Tear
Overuse injury of any of the rotator cuff tendons; supraspinatus, infraspinatus, teres minor, or subscapularis, that can result in inflammation, degeneration, and weakness that can predispose the tendon to tear. Common treatments are physical therapy, corticosteroid injection, oral anti-inflammatories, and rest.
- Rotator Cuff Tendinitis – Is an acute inflammatory response to overuse that often results in pain, swelling, weakness, and decreased function. This is usually treated with oral, anti-inflammatories, ice, rest and in some cases, steroid injections.
- Rotator Cuff Tendinosis – Is often a progression of tendinitis when your body stops the acute inflammatory response, but you still have pain, weakness, decreased function, and progression of degenerative changes. Non-steroidal anti-inflammatories (NSAIDs) such as ibuprofen are often prescribed for both tendinitis and tendinosis. A study described below supports increasing evidence that NSAID usage may interfere with the healing process and be detrimental in tendinopathy. Many papers show corticosteroids lead to soft tissue damage, cell death and tendon atrophy, reduced bone mineral density, inhibit collagen synthesis, and atrophy of muscles/skin.
Root Cause of Rotator Cuff Tendinopathy
The rotator cuff consists of 4 tendons; supraspinatus, infraspinatus, teres minor and subscapularis, that all functions to help stabilize the shoulder while allowing the arms to move through a full range of motion. The shoulder is a ball and socket joint that has a significant range of motion that can put a lot of stress on the rotator cuff tendons predisposing them to injuries. Injuries are common in anyone doing a lot of overhead movements such as tennis players, swimmers, and baseball pitchers. This is also a common injury in reaching into the backseat of the car or weight lifting.
- Rotator Cuff Tendinopathy is the result of your shoulder weakening due to chronic overuse causing damage to the shoulder tendons and ligaments.
- Rotator Cuff Tendinopathy results from shoulder instability of tendons and ligament surrounding the shoulder.
- Instability of a joint results in chronic inflammatory responses leading to a degeneration of cartilage and joint space narrowing.
- If healing does not occur as the injury or instability continue our bodies will continue compensating by increasing calcium deposits leading to bone spurs, further inflammatory responses and degeneration.
Rotator Cuff Tears
As discussed the rotator cuff tendons are easily injured due to the sheer force put on them by regular shoulder movement. The incidence of partial-thickness tears is over 30% after 40 years old. Partial-thickness tears are often more painful than full-thickness tear, which could be due to still having the ability for some movement. Injuries are common among athletes, and as noted after 40 years old. Tears are often a result of either instability as we discussed or impingement from the acromion on the supraspinous. Shoulder injuries are often not isolated and thorough exam and treatment are required for a full recovery.
Regenerative Medicine and Rotator Cuff Injuries
Regenerative medicine is an ideal therapy to heal and restore damaged areas of tendons, ligaments, and bones. Regenerative injection therapies stimulate the body’s healing process by signaling growth factors, immune cells, collagen-building precursors, and stem cells to migrate to an area of injury. Stem cells have the ability to increase fibrocartilage formation. This is the tissue that helps make up ligaments, tendons, and cartilage.
There is a growing body of research demonstrating dextrose prolotherapy, platelet-rich plasma and mesenchymal stem cell therapy are potentially effective therapies to enhance rotator cuff healing and preventing further damage and eventual arthritis.
“Rotator cuff disease has been a significant focus of research activity in recent years, as clinicians face the challenge of poor tendon healing and irreversible changes associated with rotator cuff arthropathy. Future treatment modalities involving biologics and tissue engineering hold further promise to improve outcomes for patients suffering from shoulder pathologies.”
- Killian ML, Cavinatto L, Galatz LM, Thomopoulos S. Recent advances in shoulder research. Arthritis Res Ther. 2012;14(3):214. Published 2012 Jun 15. doi:10.1186/ar3846
Summary of Treatment Options for Rotator Cuff Injuries:
- Prolotherapy injections are indicated to help strengthen tendons and ligaments to improve joint stability. This therapy can be combined with physical therapy for further strengthening of surrounding muscles and appropriate ergonomics.
- Platelet Rich Plasma therapy involves using your own blood plasma and platelets as an enriched source of growth factors, immune cells to stimulate healing of bone and soft tissue. PRP has been shown to modulate the repair and regeneration of damaged connective tissue and delay further degeneration of connective tissue. PRP is a great therapy for partial tears and moderate arthritis.
- Stem cell therapy may be an alternative for full-thickness tears if surgical intervention is not indicated. There is promising research that stem cell therapy with surgical intervention yields positive outcomes. It is important to note that full-thickness tears like all diagnoses should be based on history, physical exam, and imaging.
- Extracorporeal Shockwave Therapy (ESWT) has been shown in studies to treat tendonitis or partial thickness tears in the rotator cuff tendons before proceeding to arthroscopic intervention.
- Arthroscopic surgery to remove tissue should be considered depending on the severity and location of bone spurs.
- Some studies indicate that arthroscopic surgical repair for partial rotator cuff tears results in outcomes no better than treatment with exercise or physical therapy alone.
- Subacromial decompression should be considered depending on the anatomy of acromion and the extent of impingement if involved with rotator cuff injury.
- Rotator Cuff Full-Thickness Tear may require surgical repair as well as the removal of tissue if significant atrophy or degeneration. It is important to note that full-thickness tears like all diagnoses should be based on history, physical exam, and imaging.
- There are many factors when considering rotator cuff surgical repair and it should not be taken lightly. Rotator cuff repair can be clinically successful when performed well and rehabilitated properly. However, one study referenced below found 10 to70% percent of rotator cuff repairs form a recurrent defect after surgery. Another study found between 30% and 94% of rotator cuff repairs result in failure.
Research Studies and References
Oral Ibuprofen Interferes With Cellular Healing Responses in a Murine Model of Achilles Tendinopathy
- Bittermann A, Gao S, Rezvani S, et al. Oral Ibuprofen Interferes with Cellular Healing Responses in a Murine Model of Achilles Tendinopathy. J Musculoskelet Disord Treat. 2018;4(2):049. doi:10.23937/2572-3243.1510049
- Purpose: The attempted healing of tendon after acute injury (overloading, partial tear or complete rupture) proceeds via the normal wound healing cascade involving hemostasis, inflammation, matrix synthesis and matrix remodeling. Depending on the degree of trauma and the nature of the post-injury milieu, a variable degree of healing and recovery of function occurs. Post-injury analgesia is often achieved with NSAIDs such as Ibuprofen, however there is increasing evidence that NSAID usage may interfere with the healing process. This study aimed to investigate the cellular mechanism by which IBU therapy might lead to a worsening of tendon pathology.
- Conclusion: We conclude that the use of Ibuprofen for pain relief during inflammatory phases of tendinopathy, might interfere with the normal processes of extracellular matrix remodeling and cellular control of expression of inflammatory and wound healing genes. It is proposed that the known COX2-mediated anti-inflammatory effect of ibuprofen has detrimental effects on the turnover of a pro-inflammatory HA matrix produced in response to soft-tissue injury, thus preventing the switch to cellular responses associated with functional matrix remodeling and eventual healing.
Effectiveness of Dextrose Prolotherapy for Rotator Cuff Tendinopathy: A Systematic Review
- Catapano M, Zhang K, Mittal N, Sangha H, Onishi K, de Sa D. Effectiveness of Dextrose Prolotherapy for Rotator Cuff Tendinopathy: A Systematic Review. PM R. 2020;12(3):288–300. doi:10.1002/pmrj.12268
- Purpose: To systematically review and evaluate the efficacy and complication profile of prolotherapy using hyperosmolar dextrose solution injection for rotator cuff tendinopathy. Studies analyzed a total of 272 participants
- Conclusions: Prolotherapy with hyperosmolar dextrose solution is a potentially effective adjuvant intervention to physical therapy for patients with rotator cuff tendinopathy ranging from tendinosis to partial-thickness and small full-thickness tears. Further studies are necessary to determine effects in subpopulations as well as optimal technique including dextrose concentration, volume, and location.
Dextrose Prolotherapy Versus Control Injections in Painful Rotator Cuff Tendinopathy
- Bertrand H, Reeves KD, Bennett CJ, Bicknell S, Cheng AL. Dextrose Prolotherapy versus Control Injections in Painful Rotator Cuff Tendinopathy. Arch Phys Med Rehabil. 2015 Aug 21. pii: S0003-9993(15)01091-6
- Purpose: To compare the effect of dextrose prolotherapy on pain levels and degenerative changes in painful rotator cuff tendinopathy against 2 potentially active control injection procedures.
- Conclusions: In participants with painful rotator cuff tendinopathy who receive physical therapy, injection of hypertonic dextrose on painful entheses resulted in superior long-term pain improvement and patient satisfaction compared with blinded saline injection over painful entheses, with intermediate results for entheses injection with saline. These differences could not be attributed to a regenerative effect. Dextrose prolotherapy may improve on the standard care of painful rotator cuff tendinopathy for certain patients.
Comparative Outcomes of Extracorporeal Shockwave Therapy for Shoulder Tendinitis or Partial Tears of the Rotator Cuff in Athletes and Non-Athletes: Retrospective Study
- Chou WY, Wang CJ, Wu KT, Yang YJ, Cheng JH, Wang SW. Comparative outcomes of extracorporeal shockwave therapy for shoulder tendinitis or partial tears of the rotator cuff in athletes and non-athletes: Retrospective study. Int J Surg. 2018;51:184–190. doi:10.1016/j.ijsu.2018.01.036
- Background: Refractory shoulder tendinitis or partial thickness rotator cuff tears (PTRCTs) are common findings in overhead athletes. Previous studies have examined the effectiveness of extracorporeal shockwave therapy (ESWT) for shoulder tendinitis.
- Conclusion: The results showed ESWT was equally effective treatment in both AG and NAG. In light of its efficacy and less-invasive nature, we suggest ESWT can be used to treat athletes with refractory tendinitis or PTRCTs before proceeding to arthroscopic intervention.
Effects of Bone Marrow Aspirate Concentrate and Platelet-Rich Plasma on Patients With Partial Tear of the Rotator Cuff Tendon
- Kim SJ, Kim EK, Kim SJ, Song DH. Effects of bone marrow aspirate concentrate and platelet-rich plasma on patients with partial tear of the rotator cuff tendon. J Orthop Surg Res. 2018;13(1):1. Published 2018 Jan 3. doi:10.1186/s13018-017-0693-x
- Purpose: We compared the clinical course of rotator cuff tears between rotator cuff exercise and bone marrow aspirate concentration (BMAC)-platelet rich plasma (PRP) injection to identify the therapeutic effects of BMAC-PRP on partial tear of the rotator cuff tendon. Twenty-four patients with partial tear of the rotator cuff tendon participated in this study.
- Conclusions: BMAC-PRP improved pain and shoulder function in patients with partial tear of the rotator cuff tendon.
Failure With Continuity in Rotator Cuff Repair “Healing”
- McCarron JA, Derwin KA, Bey MJ, et al. Failure with continuity in rotator cuff repair “healing”. Am J Sports Med. 2013;41(1):134–141. doi:10.1177/0363546512459477
- Purpose: To measure the prevalence, timing, and magnitude of tendon retraction after rotator cuff repair and correlate these outcomes with formation of a full-thickness recurrent tendon defect on magnetic resonance imaging, as well as clinical outcomes.
- Conclusion: Early tendon retraction, but not the total magnitude, correlates with formation of a recurrent tendon defect and worse clinical outcomes. “Failure with continuity” (tendon retraction without a recurrent defect) appears to be a common phenomenon after rotator cuff repair. These data suggest that repairs should be protected in the early postoperative period and repair strategies should endeavor to mechanically and biologically augment the repair during this critical early period.
Impingement is one of the most common reasons for pain in the shoulder most often occurring where the top of the shoulder blade (acromion) meets the supraspinatus tendon. Shoulder impingement can be caused by repetitive overhead use, shoulder instability, osteoarthritis in the shoulder joints, tendinopathy, or anatomical variants.
Common symptoms include a slow onset of shoulder pain, especially when lifting the arm out to the side and out in front of you. Often the pain is experienced around the tip of the shoulder. Pain often improves with rest and decreasing overhead activities.
Impingement problems can occur during activities that require excessive overhead arm motion. Medical care should be sought immediately for inflammation in the shoulder because it could eventually lead to a more serious injury.
Treatments are usually conservative and consist of physical therapy, nonsteroidal anti-inflammatory medications (NSAIDs), and cortisone (steroid) injections. Surgical interventions may be necessary if anatomical variants are the root cause of impingement.
- Studies have shown that subacromial decompression (surgery) for impingement injuries do not provide clinical benefits over placebo in pain, function or health-related quality of life.
- Studies have also shown that surgery plus physical therapy compared to physical therapy alone have the same outcomes when comparing the improvement of pain and function.
Regenerative Medicine for Impingement Injuries
Impingement injuries can often be a result of instability of tendons (Rotator Cuff) and/or ligaments supporting the shoulder that allow for increased movement so the bone will impinge the tendon. Prolotherapy is an excellent treatment for this condition. Prolotherapy uses a dextrose based solution to create an inflammatory response recruiting fibroblast, growth factors, and even stem cells to an area of injury. In turn, this helps stimulate repair of tissues reinforcing connective tissue resulting in ligament/tendon strengthening and stability.
- One study looked at the effects of dextrose injection in patients with chronic shoulder pain caused by subacromial impingement syndrome. The study demonstrated significant improvement in pain and function scores as well as continual improvement in range of motion for 6 months following treatment.
- Another small study found 20 of 31 patients with chronic moderate-to-severe shoulder pain due to impingement and/or arthritis reported substantial pain reduction and no adverse events with ultrasound-guided prolotherapy dextrose solution. Studies cited below.
- Platelet-rich plasma (PRP) therapy involves using your own blood plasma and platelets as an enriched source of growth factors, immune cells, and collagen-building precursors to stimulate healing of bone and soft tissue. PRP is a more aggressive form of prolotherapy that places the growth factors and immune cells at the site of injury instead of the body needing to bring them to the site of injury. PRP is great for tears, shoulder osteoarthritis, and cartilage lesions.
- Platelet-rich plasma applied in the subacromial space in patients with shoulder impingement syndrome showed improvement in pain and daily activities. Study cited below.
It is important to note that treatment regardless of the solution should address the whole shoulder. Proper physical exam, history, and imaging should determine all structures involved that need to be treated to help address issues of rotator cuff weakness and shoulder instability.
Research Studies and References
Treatment of the Shoulder Impingement Syndrome With PRP Injection
Šmíd P, Hart R, Komzák M, Paša L, Puskeiler M. Léčba impingement syndromu ramena pomocí injekce PRP [Treatment of the Shoulder Impingement Syndrome with PRP Injection]. Acta Chir Orthop Traumatol Cech. 2018;85(4):261–265.
Purpose: This study aimed to explore the effects of new therapeutic procedures in patients with shoulder impingement syndrome. The primary goal of the study was to confirm the hypothesis that the application of the platelet-rich plasma (PRP) in patients with shoulder impingement syndrome will have a positive effect on both the subjective and objective evaluation of their condition.
Conclusions: Based on the results of our study, the hypothesis can be accepted that the concentrate of platelet-rich plasma administered through a series of 3 injections applied in the subacromial space in patients with shoulder impingement syndrome has positive effects on the daily activities of patients as well as on the objective evaluation via the selected scoring systems.
Subacromial Decompression Surgery for Rotator Cuff Disease
Karjalainen TV, Jain NB, Page CM, et al. Subacromial decompression surgery for rotator cuff disease. Cochrane Database Syst Rev. 2019;1(1):CD005619. Published 2019 Jan 17. doi:10.1002/14651858.CD005619.pub3
Background: Surgery for rotator cuff disease is usually used after non-operative interventions have failed, although our Cochrane Review, first published in 2007, found that there was uncertain clinical benefit following subacromial decompression surgery.
Conclusions: The data in this review do not support the use of subacromial decompression in the treatment of rotator cuff disease manifest as painful shoulder impingement. High-certainty evidence shows that subacromial decompression does not provide clinically important benefits over placebo in pain, function or health-related quality of life.
The effectiveness of surgical vs conservative interventions on pain and function in patients with shoulder impingement syndrome. A systematic review and meta-analysis
Nazari G, MacDermid JC, Bryant D, Athwal GS. The effectiveness of surgical vs conservative interventions on pain and function in patients with shoulder impingement syndrome. A systematic review and meta-analysis. PLoS One. 2019;14(5):e0216961. Published 2019 May 29. doi:10.1371/journal.pone.0216961
Objective: To assess the effectiveness of surgical vs conservative interventions on pain and function in patients with subacromial impingement syndrome.
Conclusion: The effects of surgery plus physiotherapy compared to physiotherapy alone on improving pain and function are too small to be clinically important at 3-, 6-months, 1-, 2-, 5- and ≥ 10-years follow up.
The Effects of Prolotherapy in Patients With Subacromial Impingement Syndrome
Hannan EA, Gulseren Sr A, Hysenaj N. The Effects of Prolotherapy in Patients With Subacromial Impingement Syndrome. In ARTHRITIS AND RHEUMATISM 2013 Oct 1 (Vol. 65, pp. S461-S462). 111 RIVER ST, HOBOKEN 07030-5774, NJ USA: WILEY-BLACKWELL.
Background/Purpose: Recent treatments for subacromial impingement syndrome (SIS) are palliative. Dextrose injection which is called prolotherapy has emerged as a treatment option for chronic situations such as tendinitis and bursitis. The aim of the study is to investigate the effects of dextrose injection in patients with chronic shoulder pain caused by subacromial impingement syndrome.
Conclusion/Results: There were no adverse events reported. The study demonstrated significant improvement in pain and function scores in both injection groups, Prolotherapy and lidocaine. Shoulder flexion, abduction, internal and external rotations showed significant improvements in both groups in the first 3 months. However, while the range of shoulder flexion did not improve in the control group during the last three months, this range of motion continued to improve significantly in treatment group (prolotherapy group) over the same period.
Ultrasound-Guided Prolotherapy for Acromial Enthesopathy and Acromioclavicular Joint Arthropathy: A Single-Arm Prospective Study
Hsieh PC, Chiou HJ, Wang HK, Lai YC, Lin YH. Ultrasound-Guided Prolotherapy for Acromial Enthesopathy and Acromioclavicular Joint Arthropathy: A Single-Arm Prospective Study. J Ultrasound Med. 2019;38(3):605–612. doi:10.1002/jum.14727
Objective/Purpose: Prolotherapy is an injection-based complementary treatment for various musculoskeletal diseases. The aim of this study was to evaluate the therapeutic efficacy of ultrasound-guided prolotherapy in the treatment of acromial enthesopathy and acromioclavicular joint arthropathy.
Results/Conclusion: Twenty of the 31 patients reported substantial pain reduction without adverse effects after the intervention. It was determined ultrasound-guided prolotherapy with a 15% dextrose solution is an effective and safe therapeutic option for moderate-to-severe acromial enthesopathy and acromioclavicular joint arthropathy.
Bicep tendinopathies and tears occur as a result of chronic microtrauma or acute traumatic injury to the long head of the biceps tendon. Common presentations are upper arm/shoulder pain that may radiate into the upper arm. Chronic microtrauma in sports with overhead actions such as tennis, baseball, and swimming results in inflammation, swelling, and pain that may progress to thickening of the tendon with loss of integrity. Loss of integrity can result in the tendon being more vulnerable to tearing.
Biceps injuries often accompany rotator cuff injuries, but can also be associated with shoulder arthritis, glenohumeral ligaments lesions, SLAP tears, and subacromial impingement syndrome.
Conservative treatments include rest, non-steroidal anti-inflammatories NSAIDs, and physical therapy. Surgery may be indicated depending on the severity of the tears. Something that should be taken into consideration regarding treatments is that there is increasing evidence that NSAID usage may interfere with the healing process and be detrimental in tendinopathy. Many papers show corticosteroids lead to soft tissue damage, cell death, and tendon atrophy.
Regenerative Medicine and Bicep Injuries
- Platelet Rich Plasma (PRP) seems to enhance angiogenesis (improved blood supply) which may accelerate the healing process.
- Platelet Rich Plasma (PRP) treatment can enhance tendon healing because it promotes activation and differentiation of tendon stem cells.
- Studies have demonstrated that PRP can increase both the number of cells and the cellular component by enhancing fibroblast proliferation and collagen production, and thus strengthen healed tendons and ligament. These showed that PRP improved not only collagen production in tendons but also their tensile strength and decreased scar tissue formation.
- Extracorporeal Shockwave Therapy (ESWT) has been shown in studies to treat tendonitis or partial thickness tears in the rotator cuff tendons before proceeding to arthroscopic intervention.
- A large number of studies have demonstrated the beneficial effects of PRP on the healing of tendons and ligaments at the molecular, cellular, animal, and human trail levels.
Research Studies and References
The Influence of Platelet-Rich Plasma on Angiogenesis During the Early Phase of Tendon Healing
- Lyras DN, Kazakos K, Verettas D, et al. The influence of platelet-rich plasma on angiogenesis during the early phase of tendon healing. Foot Ankle Int. 2009;30(11):1101–1106. doi:10.3113/FAI.2009.1101
- Background: The poor vascularity of tendons is a major factor in their limited healing capacity. The aim of this study was to assess the effect of Platelet Rich Plasma (PRP) on angiogenesis during tendon healing.
- Conclusion: PRP seems to enhance neovascularization which may accelerate the healing process and promote scar tissue of better histological quality.
- Clinical relevance: Although these results need replication and further biomechanical research, PRP may promote tendon healing acceleration.
Platelet-rich Plasma Releasate Promotes Differentiation of Tendon Stem Cells Into Active Tenocytes
- Zhang J, Wang JH. Platelet-rich plasma releasate promotes differentiation of tendon stem cells into active tenocytes. Am J Sports Med. 2010;38(12):2477–2486. doi:10.1177/0363546510376750
- Background: Platelet-rich plasma (PRP) has been used to enhance tendon healing in clinical settings. However, the cellular mechanisms underlying PRP treatment of injured tendons remain unclear. The aim of this study was to determine the effects of PRP, in the form of PRP-clot releasate (PRCR), on tendon stem cells (TSCs), a newly discovered cell population in tendons.
- Conclusion: The PRCR treatment promotes differentiation of TSCs into active tenocytes exhibiting high proliferation rates and collagen production capability.
- Clinical relevance: The findings of this study suggest that PRP treatment of injured tendons is “safe” as it promotes TSC differentiation into tenocytes rather than nontenocytes, which would compromise the structure and function of healing tendons by formation of nontendinous tissues. Moreover, they suggest that PRP treatment can enhance tendon healing because tenocytes induced to differentiate by PRP are activated to proliferate quickly and produce abundant collagen to repair injured tendons that have lost cells and matrix.
Augmenting tendon and ligament repair with platelet-rich plasma (PRP)
- Yuan T, Zhang CQ, Wang JH. Augmenting tendon and ligament repair with platelet-rich plasma (PRP). Muscles Ligaments Tendons J. 2013;3(3):139–149. Published 2013 Aug 11.
- Background: Tendon and ligament injuries (TLI) commonly occur in athletes and non-athletes alike, and remarkably debilitate patients’ athletic and personal abilities. Current clinical treatments, such as reconstruction surgeries, do not adequately heal these injuries and often result in the formation of scar tissue that is prone to re-injury. Platelet-rich plasma (PRP) is a widely used alternative option that is also safe because of its autologous nature. PRP contains a number of growth factors that are responsible for its potential to heal TLIs effectively.
- Conclusion: Overall, PRP treatment has an excellent safety record in clinical applications. The adverse effects reported are minimal. A large number of studies have demonstrated the beneficial effects of PRP on the healing of tendons and ligaments at the molecular, cellular, animal, and human trail levels, but the efficacy of PRP treatment for TLIs is still controversial in orthopaedics and sports medicine fields. This situation may be attributed to the complexity and diversity of PRP preparations used in these studies. For this, several factors require optimization, including compositional variations in PRP preparations and the dosage used in treatments, among others.
Comparative Outcomes of Extracorporeal Shockwave Therapy for Shoulder Tendinitis or Partial Tears of the Rotator Cuff in Athletes and Non-Athletes: Retrospective Study
- Chou WY, Wang CJ, Wu KT, Yang YJ, Cheng JH, Wang SW. Comparative outcomes of extracorporeal shockwave therapy for shoulder tendinitis or partial tears of the rotator cuff in athletes and non-athletes: Retrospective study. Int J Surg. 2018;51:184–190. doi:10.1016/j.ijsu.2018.01.036
- Background: Refractory shoulder tendinitis or partial thickness rotator cuff tears (PTRCTs) are common findings in overhead athletes. Previous studies have examined the effectiveness of extracorporeal shockwave therapy (ESWT) for shoulder tendinitis.
- Conclusion: The results showed ESWT was equally effective treatment in both AG and NAG. In light of its efficacy and less-invasive nature, we suggest ESWT can be used to treat athletes with refractory tendinitis or PTRCTs before proceeding to arthroscopic intervention.
Arthritis can affect both joints of the shoulder the acromioclavicular joint (AC) this is where the clavicle meets the top of the shoulder blade (acromion) or at the glenohumeral joint this is where the head of the humerus (top of the arm bone) sits in the scapula (shoulder blade).
Arthritis of the shoulder joint is usually secondary to trauma such as a shoulder separation or chronic wear and tear from extensive use and range of motion predisposing to joint instability. Chronic joint instability leads to degrading enzymes trying to clean up the inflammatory debris, weakening of collagen networks supporting the shoulder, cartilage degeneration, joint space narrowing, cyst formation, and osteophyte formation.
Common symptoms are pain, swelling, decreased range of motion, clicking and catching.
Treatments are usually conservative and consist of physical therapy, nonsteroidal anti-inflammatory medications (NSAIDs), and cortisone (steroid) injections. The problem with these treatments is that cortisone shots and anti-inflammatory drugs have been shown to yield temporary pain benefit, while long-term use results in loss of function and even more chronic pain by inhibiting the healing process of soft tissues and accelerating cartilage degeneration.
Regenerative Medicine as a Treatment for Arthritis
Regenerative medicine injections stimulate the body’s natural immune response, an inflammatory response, encouraging growth factors, fibroblast, immune cells and collagen-building precursors to the injured area to promote healing and repair.
- Platelet-rich plasma (PRP) therapy involves using your own blood plasma and platelets as an enriched source of growth factors, immune cells, and collagen-building precursors to stimulate healing of bone and soft tissue. PRP has been shown to modulate the repair and regeneration of damaged articular cartilage in the joints and delay further degeneration of cartilage. Studies have replicated reduction in pain, decreased inflammation in the joint space, and improvement in the quality of life scores.
- Autologous stem cell (from your own body) therapies using both mesenchymal stromal cells (MSCs) and hematopoietic stem cells have shown therapeutic potential for advanced osteoarthritis. In orthopedic injuries and degeneration, stem cells have the potential to signal for the repair of damaged tissue with possible regeneration of tissue. It is important to note that research is mixed with regard to whether regenerative medicine truly regenerates tissue. What does seem to be more reproducible are a decrease in further degenerative changes, pain, and improved function.
Regenerative Medicine does not work for everyone and there are many variables to be considered when choosing what treatment is right for you. Differences in PRP concentrations, PRP preparation methods, source of stem cells, injection techniques, accurate diagnosis, determination of pain generators, conjunction with other therapies from everything to different injection therapies to physical therapy. It should not be underestimated the importance of treating whole-body inflammation and optimizing immune function in order to get the best results from treatments. All of these should be considered and I believe comprehensive treatments lead to optimal healing.
Research Studies and References
“The therapeutic potential of mesenchymal stromal cells (MSCs) is evident by the number of new and ongoing trials targeting an impressive variety of conditions.”
- Heldring N, Mäger I, Wood MJ, Le Blanc K, Andaloussi SE. Therapeutic Potential of Multipotent Mesenchymal Stromal Cells and Their Extracellular Vesicles. Hum Gene Ther. 2015;26(8):506–517. doi:10.1089/hum.2015.072
Does Intra-articular Platelet-Rich Plasma Injection Provide Clinically Superior Outcomes Compared With Other Therapies in the Treatment of Knee Osteoarthritis? A Systematic Review of Overlapping Meta-analyses
- Campbell KA, Saltzman BM, Mascarenhas R, et al. Does Intra-articular Platelet-Rich Plasma Injection Provide Clinically Superior Outcomes Compared With Other Therapies in the Treatment of Knee Osteoarthritis? A Systematic Review of Overlapping Meta-analyses. Arthroscopy. 2015;31(11):2213–2221. doi:10.1016/j.arthro.2015.03.041
- Purpose: The aims of this study were (1) to perform a systematic review of meta-analyses evaluating platelet-rich plasma (PRP) injection in the treatment of knee joint cartilage degenerative pathology
- Conclusions: IA-PRP is a viable treatment for knee OA and has the potential to lead to symptomatic relief for up to 12 months. There appears to be an increased risk of local adverse reactions after multiple PRP injections. IA-PRP offers better symptomatic relief to patients with early knee degenerative changes, and its use should be considered in patients with knee OA.
The labrum makes up the articular surface of the shoulder joint. It is a ring of fibrous cartilage that lines the cavity of the scapula (shoulder blade) and where the humerus (the bone in the upper arm) sits. Injuries to the labrum can be from chronic microtrauma due to repetitive shoulder motion for an acute injury.
Labral tears are common after falls with an outstretched hand or a hard hit to the shoulder resulting in dislocation. Injuries resulting in labral tear may be associated with a biceps tendon injury and/or rotator cuff injury. Symptoms include pain after trauma, difficulty performing activities of daily living including hair combing, shaving, and eating, and/or pain with activities such as throwing, swimming, and rowing.
Treatments are usually conservative and consist of physical therapy, Nonsteroidal anti-inflammatory medications (NSAIDs), and cortisone (steroid) injections. The problem with these treatments is that cortisone shots and anti-inflammatory drugs have been shown to yield temporary pain benefit, while long-term use results in loss of function and even more chronic pain by inhibiting the healing process of soft tissues and accelerating cartilage degeneration.
The type of labral tear and other structures involved are all factors that need to be assessed to determine if surgery is indicated. That being said shoulder surgery is not something to be taken lightly. Each case of a suspected labral lesion must be evaluated on an individualized basis.
A study done by A Norwegian research team lead by Dr. Cecilie Piene Schrøder, an Orthopedic surgeon conducted a double-blind, randomized, sham-controlled trial with 118 surgical candidates. The group divided the participants into treatments between sham surgery, biceps tendinosis, and labral repair. No significant differences in results between the groups were found. Citation below.
“Labral injuries can result in instability of tendons and ligaments supporting the shoulder.”
Injuries to the labrum and surrounding tendons and ligaments from chronic wear and tear or movements where the joint is forced out of its normal position can result in shoulder joint instability. This can lead to pain during movements such as raising the arm, feelings that the shoulder is moving out of its socket, and dislocation of one of the joints in the shoulder. Prolotherapy is an excellent treatment for joint instability.
Regenerative Medicine as a Treatment for Labral Tears
Regenerative medicine injections stimulate the body’s natural immune response, an inflammatory response, encouraging growth factors and immune cells to the injured area to promote healing and repair. Regenerative medicine injections consist of prolotherapy, platelet-rich plasma, and stem cells.
- Prolotherapy uses a dextrose based solution to create an inflammatory response recruiting fibroblast, growth factors, and even stem cells to an area of injury. In turn, this helps stimulate repair of tissues reinforcing connective tissue resulting in ligament/tendon strengthening and stability.
- Platelet-rich plasma (PRP) therapy involves using your own blood plasma and platelets as an enriched source of growth factors, immune cells, and collagen-building precursors to stimulate healing of bone and soft tissue. PRP is a more aggressive form of prolotherapy that places the growth factors and immune cells at the site of injury instead of the body needing to bring them to the site of injury. PRP is great for tears, shoulder osteoarthritis, and cartilage lesions.
- Autologous stem cell (from your own body) therapies using both mesenchymal stromal cells (MSCs) and hematopoietic stem cells have shown therapeutic potential for advanced injuries. In orthopedic injuries and degeneration, stem cells have the potential to signal for the repair of damaged tissue with possible regeneration of tissue. It is important to note that research is mixed with regard to whether regenerative medicine truly regenerates tissue. What does seem to be more reproducible are a decrease in further degenerative changes, pain, and improved function.
Research Studies and References
SLAP lesions, An Opinion Piece
- Schrøder CP. SLAP lesions, An Opinion Piece. Open Orthop J. 2018;12:342–345. Published 2018 Jul 31. doi:10.2174/1874325001812010342
- Objective: To conduct a clinical trial in which 118 patients with a mean age of 40 years were randomized to labral repair, biceps tenodesis or sham (placebo) surgery. We stated that to obtain Level I or II evidence, randomized studies designed to compare SLAP repair, biceps tenodesis and non-operative treatment were needed.
- Results: The results showed significant improvement in both subjective and objective scores for all three groups, but surprisingly, no significant group differences in the intention to treat analysis. No significant differences in results between the groups were found
Prolotherapy: A Non-Invasive Approach to Lesions of the Glenoid Labrum
- Hauser RA, Dolan E, Orlofsky A. Prolotherapy: A Non-Invasive Approach to Lesions of the Glenoid Labrum; A Non-Controlled Questionnaire Based Study. The Open Rehabilitation Journal. 2013 Dec 27;6(1).
- Background: Management of patients with glenohumeral joint disorders generally includes a recommended period of conservative treatment in an attempt to avoid arthroscopic surgery. There is little data available, however, with respect to the efficacy of conservative treatment, and guidelines for the design of non-operative treatment plans have not been developed. While arthroscopic treatment of glenoid labral tears produces good to excellent outcomes in most patients, the likelihood of success can vary with patient characteristics, including age and physical activity. These limitations, combined with the expense and potential complications of arthroscopic therapy, suggest a need for further investigation of non-operative treatment modalities. Here we review relevant aspects of glenoid labral tear and describe initial observations in a group of patients treated with regenerative injection (prolotherapy) for labral tears.
- Conclusion: Uncertainties in the management of glenoid labral lesions, in particular with respect to the efficacy of conservative treatments, provide a rationale for the investigation of regenerative injection therapy for labral tear. Our initial experience with hypertonic dextrose in patients with glenoid labral tear suggests that the procedure is safe and potentially efficacious. We observed substantial gains in pain relief and functionality in a large majority of patients
Dr. Squires takes a passionate approach to her work. She is genuinely concerned for the well being of the patients under her care. Her prolo therapy helped my shoulder greatly. She also cured other ailments in our family. Highly recommended.
