Natural Hip Pain Relief
The hip joint is the largest weight-bearing joint in the human body. The hip joint consists of the thighbone or femur, which joins the pelvis at a deep socket called the acetabulum. The hip joint is a ball and socket joint meaning it allows multidirectional movement and is supported by multiple muscles, ligaments and tendons. Because the hip joint is the largest weight-bearing joint and does allow for multidirectional movement it is vulnerable to injury especially “wear and tear” or degenerative disease that adversely affect the joint’s range of motion and the ability to bear weight.
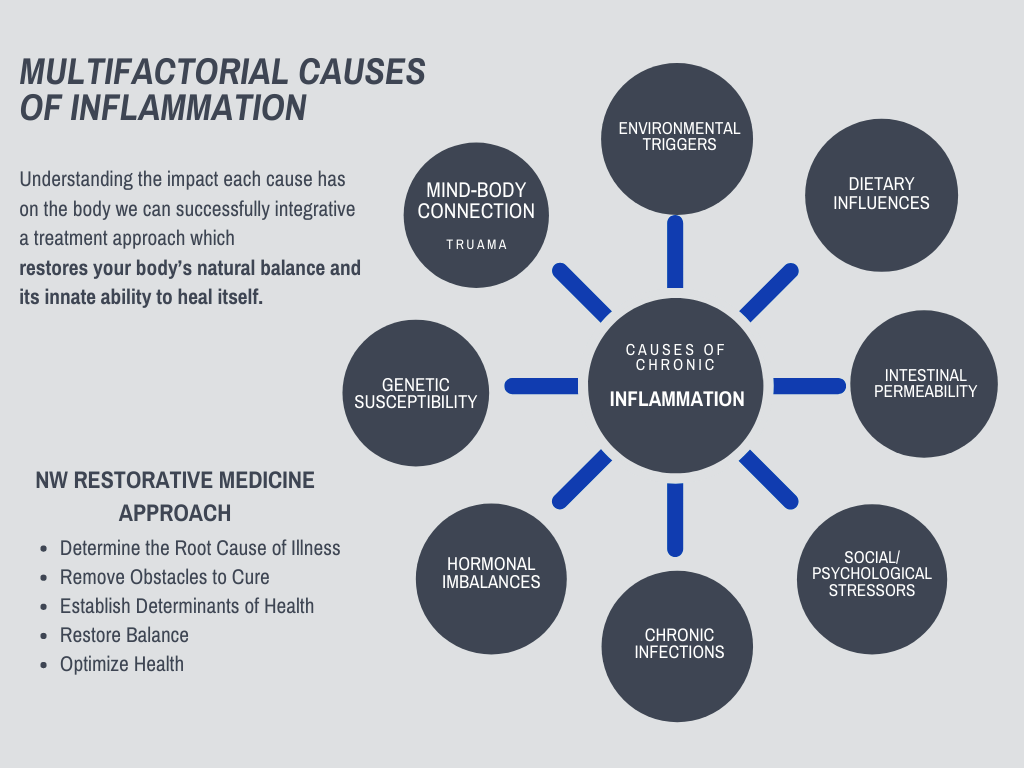
Your Hip is Connected to Your Whole Body, and so is Your Pain and Inflammation
As a result, the cause of hip pain and inflammation comes from many factors, requiring a whole-body approach to relieving pain.
Dr. Squires’ approach brings together a holistic treatment of all the factors contributing to your chronic inflammation and pain. Personalizing treatment to the factors most impacting your source of pain.
And combines it with a Regenerative Medicine approach that stimulates your own body’s healing response naturally.
Regenerative medicine is a cell-based therapy using advanced scientific techniques in the treatment of degenerative disease, orthopedic injuries, and joint conditions.
Discover how Dr. Squires can help by scheduling an initial consult »
The common hamstring tendon attaches the sits bone (ischium of the pelvis) to the lower leg bone (tibia). Hamstring tendinosis is usually due to chronic repetitive microtrauma during sports such as long-distance running, sprinting or jumping as well as sports with burst of speed from forceful takeoff or requiring forward swing of the leg. Tendinopathy is a result of an inflammatory response to overuse that often results in pain, swelling, weakness, and decreased function. The continual inflammatory response can lead to degenerative changes, decrease blood supply, disorganization of tendon fibers, and a failed healing response.
Individuals will experience pain while sitting, pain and tightness with forward kicking or hamstring stretching or feeling a constant pulling at the insertion of the tendon located at the sits bone.
Treatments usually are conservative with rest, physical therapy, non-steroidal anti-inflammatories (NSAIDs) such as ibuprofen/Advil or steroid injections. NSAID use is controversial due to increasing evidence that NSAID usage may interfere with the healing process and be detrimental in tendinopathy. Many papers show corticosteroids lead to soft tissue damage, cell death, and tendon atrophy.
It is important to find the root cause of hamstring or buttock pain. The root cause could be an isolated injury of the hamstring as discussed above. It could also be associated with low back pain from the lumbar spine, a sacroiliac injury, a hip joint injury such as a labral tear or even a knee injury because the hamstring crosses both the hip joint and the knee joint. All of these areas need to be evaluated for a comprehensive treatment that resolves the root cause of pain.
Regenerative Medicine and Hamstring Tendinosis
- Prolotherapy uses a dextrose based solution to create an inflammatory response recruiting fibroblast, growth factors, and even stem cells to an area of injury. In turn, this helps stimulate repair of tissues reinforcing connective tissue resulting in ligament/tendon strengthening and stability.
- Platelet Rich Plasma (PRP) involves taking your own blood and processing it to get endogenous growth factors, immune cells, and fibroblasts (precursor to connective tissue) and injecting them into the site of injury. PRP uses your own cells to facilitate healing.
- Tendon healing utilizes the cells provided by platelet-rich plasma to instigate an inflammatory response, cellular proliferation, and tissue remodeling.
- Platelet Rich Plasma (PRP) seems to enhance angiogenesis (improved blood supply) which may accelerate the healing process.
- Platelet Rich Plasma (PRP) treatment can enhance tendon healing because it promotes activation and differentiation of tendon stem cells.
- Studies have demonstrated that PRP can increase both the number of cells and the cellular component by enhancing fibroblast proliferation and collagen production, and thus strengthen healed tendons and ligament. These studies showed that PRP improved not only collagen production in tendons but also their tensile strength and decreased scar tissue formation.
- Extracorporeal Shockwave Therapy (ESWT) has been shown in studies to treat tendonitis or partial thickness tears in tendons. A study comparing the effectiveness of shockwave therapy to other non-operative treatments for chronic proximal hamstring tendinopathy found 85% improvement in pain with the individuals treated with shockwave. Study cited below.
- It should be noted that regenerative medicine efficacy remains controversial and research should continue. There are many factors that contribute to increased efficacy including processing/preparation of PRP, how much is injected, activation of PRP, injection technique, timing, number of application and timing of injections as well as comorbidities or concomitant therapies.
Research Studies and References
Platelet-rich plasma treatment improves outcomes for chronic proximal hamstring injuries in an athletic population
- Fader RR, Mitchell JJ, Traub S, et al. Platelet-rich plasma treatment improves outcomes for chronic proximal hamstring injuries in an athletic population. Muscles Ligaments Tendons J. 2015;4(4):461–466. Published 2015 Feb 5.
- Background/Purpose: Chronic proximal hamstring tendinopathies is a disabling activity related condition. Currently, there is no well-accepted or extensively documented non-operative treatment option that provides consistently successful results. The purpose of this study is to evaluate the efficacy of ultrasound guided platelet-rich plasma injections in treating chronic proximal hamstring tendinopathies.
- Conclusion: Chronic hamstring tendinopathy is a debilitating condition secondary to the pain, which limits an athlete’s ability to perform. For refractory cases of chronic insertional proximal hamstring injuries, platelet-rich plasma injections are safe and show benefit in the majority of patients in our study, allowing return to pre-injury activities. Six months after the injection, 10/18 patients had 80% or greater improvement in pain scores.
Outcomes After Ultrasound-Guided Platelet-Rich Plasma Injections for Chronic Tendinopathy: A Multicenter, Retrospective Review
- Mautner K, Colberg RE, Malanga G, et al. Outcomes after ultrasound-guided platelet-rich plasma injections for chronic tendinopathy: a multicenter, retrospective review. PM R. 2013;5(3):169–175. doi:10.1016/j.pmrj.2012.12.010
- Objective: To determine whether ultrasound-guided platelet-rich plasma (PRP) injections are an effective treatment for chronic tendinopathies.
- Conclusions: In this retrospective study, in which180 individuals were evaluated after administration of PRP for chronic tendinopathy, we found that the majority, 82%, of patients indicated moderate to complete improvement in pain symptoms.
Shockwave Therapy for the Treatment of Chronic Proximal Hamstring Tendinopathy in Professional Athletes
- Cacchio A, Rompe JD, Furia JP, Susi P, Santilli V, De Paulis F. Shockwave therapy for the treatment of chronic proximal hamstring tendinopathy in professional athletes. Am J Sports Med. 2011;39(1):146–153. doi:10.1177/0363546510379324
- Background: Chronic proximal hamstring tendinopathy is an overuse syndrome that is usually managed by nonoperative methods. Shockwave therapy has proved to be effective in many tendinopathies.
- Conclusion: Shockwave therapy is a safe and effective treatment for patients with chronic proximal hamstring tendinopathy. 85% or individuals in the shockwave group and 10% of individuals in the exercise group achieved a reduction of at least 50% in pain.
Gluteus Medias tendon is the most common tendon injured in the outer hip. Tendinopathies of gluteus medias can result from an injury, but most often from instability and overuse. Overuse and instability result in inflammation, degeneration, and weakness that can predispose the tendon to tear. Symptoms include pain and weakness on the side of the hip that can alter your gait leading to further exacerbation of symptoms.
It is often associated with trochanteric bursitis because the gluteus medias tendon attaches on the greater trochanter of the femur (thigh bone) on the outside of the hip. At the attachment, there is a bursa, which is a fluid-filled sac that cushions the tendon attachment to reduce friction and facilitate movement. The bursa can become inflamed and painful with increased instability resulting in increased rubbing at the tendon attachments. Treatment should focus on strengthening and stabilizing the tendons and muscles surrounding the hip joint as well as assessing compensation in the low back, knee and ankle.
Common treatments are physical therapy, corticosteroid injection, oral anti-inflammatories, and rest. NSAID use is controversial due to increasing evidence that NSAID usage may interfere with the healing process and be detrimental in tendinopathy. Many papers show corticosteroids lead to soft tissue damage, cell death, and tendon atrophy, and inhibit collagen synthesis.
Studies have shown greater clinical improvement and reduction in symptoms with Platelet Rich Plasma compared to Corticosteroid injections.
Hip joint and low back instability needs to be addressed to treat the root cause of gluteus medius tendinopathy and trochanteric bursitis. Ligaments and tendons can lose their tensile strength with chronic wear and tear leading to decreased stability and increased movement. Muscles will contract to try to stabilize an unstable joint, which can pull on the tendons putting more strain on them and increasing pain and inflammation leading to further damage. More muscles and connective tissue will get recruited to try and stabilize. Pain and tightness can move to the iliotibial band, piriformis, muscles in the low back, and muscles surrounding the knee.
Treatment approaches are the same for other tendons and ligament injuries. Proper alignment is crucial for stabilization and healing. I recommend physical therapy, chiropractic, and osteopathic manipulation to ensure proper movement and function with any injection therapy for gluteus medias injuries and trochanteric bursitis.
Regenerative Medicine Therapies for Gluteal Tendon and Trochanteric Bursitis
- Prolotherapy uses a dextrose based solution to create an inflammatory response recruiting fibroblast, growth factors, and even stem cells to an area of injury. In turn, this helps stimulate repair of tissues reinforcing connective tissue resulting in ligament/tendon strengthening and stability.
- Platelet Rich Plasma (PRP) involves taking your own blood and processing it to get endogenous growth factors, immune cells, and fibroblasts (precursor to connective tissue) and injecting them into the site of injury. PRP uses your own cells to facilitate healing.
- Tendon healing utilizes the cells provided by platelet-rich plasma to instigate an inflammatory response, cellular proliferation, and tissue remodeling.
- Platelet Rich Plasma (PRP) seems to enhance angiogenesis (improved blood supply) which may accelerate the healing process.
- Platelet Rich Plasma (PRP) treatment can enhance tendon healing because it promotes activation and differentiation of tendon stem cells.
- Studies have demonstrated that PRP can increase both the number of cells and the cellular component by enhancing fibroblast proliferation and collagen production, and thus strengthen healed tendons and ligament. These showed that PRP improved not only collagen production in tendons but also their tensile strength and decreased scar tissue formation.
- Extracorporeal Shockwave Therapy (ESWT) has been shown in studies to treat tendinitis or partial-thickness tears in tendons.
Research Studies and References
Leucocyte-Rich Platelet-Rich Plasma Treatment of Gluteus Medius and Minimus Tendinopathy: A Double-Blind Randomized Controlled Trial With 2-Year Follow-up
- Fitzpatrick J, Bulsara MK, O’Donnell J, Zheng MH. Leucocyte-Rich Platelet-Rich Plasma Treatment of Gluteus Medius and Minimus Tendinopathy: A Double-Blind Randomized Controlled Trial With 2-Year Follow-up. Am J Sports Med. 2019;47(5):1130–1137. doi:10.1177/0363546519826969
- Purpose: This follow-up study was conducted to determine whether there would be a sustained long-term difference in the modified Harris Hip Score (mHHS) at 2 years for a leucocyte-rich PRP (LR-PRP) injection in the treatment of chronic gluteal tendinopathy.
- Conclusion: Among patients with chronic gluteal tendinopathy and a length of symptoms >15 months, a single PRP injection performed under ultrasound guidance to the tendon results in greater improvement in pain and function than a single corticosteroid injection. The improvement after PRP injection is sustained at 2 years, whereas the improvement from a corticosteroid is maximal at 6 weeks and not maintained beyond 24 weeks.
The Effectiveness of Platelet-Rich Plasma Injections in Gluteal Tendinopathy: A Randomized, Double-Blind Controlled Trial Comparing a Single Platelet-Rich Plasma Injection With a Single Corticosteroid Injection
- Fitzpatrick J, Bulsara MK, O’Donnell J, McCrory PR, Zheng MH. The Effectiveness of Platelet-Rich Plasma Injections in Gluteal Tendinopathy: A Randomized, Double-Blind Controlled Trial Comparing a Single Platelet-Rich Plasma Injection With a Single Corticosteroid Injection. Am J Sports Med. 2018;46(4):933–939. doi:10.1177/0363546517745525
- Purpose: Gluteus medius/minimus tendinopathy is a common cause of lateral hip pain or greater trochanteric pain syndrome. This study compared a single platelet-rich plasma (PRP) injection compared with a corticosteroid injection in the treatment of gluteal tendinopathy
- Conclusion: Patients with chronic gluteal tendinopathy >4 months, diagnosed with both clinical and radiological examinations, achieved greater clinical improvement at 12 weeks when treated with a single PRP injection than those treated with a single corticosteroid injection
Long-term Outcome of Low-Energy Extracorporeal Shockwave Therapy on Gluteal Tendinopathy Documented by Magnetic Resonance Imaging
- Seo KH, Lee JY, Yoon K, et al. Long-term outcome of low-energy extracorporeal shockwave therapy on gluteal tendinopathy documented by magnetic resonance imaging. PLoS One. 2018;13(7):e0197460. Published 2018 Jul 17. doi:10.1371/journal.pone.0197460
- Background: Previous outcome studies for extracorporeal shock wave therapy (ESWT) have included clinically diagnosed greater trochanteric pain syndrome (GTPS). The purpose of this study is to investigate outcome of ESWT on GTPS with gluteal tendinopathy documented by magnetic resonance imaging (MRI).
- Conclusion: Low-energy extracorporeal shock wave therapy (ESWT) can be an effective treatment for pain relief in chronic greater trochanteric pain syndrome with MRI-documented gluteal tendinopathy. However, its long-term effect appears to decrease with time. Success rates were 83.3% (immediate) and 55.6% (long-term), respectively. Other studies have shown long term pain relief in tendinopathy.
Piriformis syndrome is inflammation of the sciatic nerve secondary to irritation or compression by the piriformis muscle. Trauma to the gluteal region is the most common cause though it can be caused by overuse such as in athletes or on the other end prolonged sitting. There can be anatomical variants of piriformis muscles where the nerve goes through the muscle increasing chances of compression. Piriformis syndrome can also be a compensation for foot instability resulting in contraction of hip muscles trying to stabilize instability. It has also been associated with sacroiliitis or hypermobility of the sacroiliac joint which is also compensation of increased contraction of hip muscles trying to stabilize an instability putting more strain on the muscle resulting in compression of the sciatic nerve.
Most common symptoms are chronic gluteal pain which radiates into lower extremity similar to L5-S1 radiculopathy. Pain is also increased by bringing the leg inwards or rotating the leg inwards.
Treatments include physical therapy, steroid injections, botox injections and anti-inflammatories.
Regenerative Medicine Treatments for Piriformis Syndrome and Sciatic Pain
- Perineural Injection Therapies – Perineural injection therapy specifically targets neuropathic pain and neurogenic inflammation meaning the nerve fiber itself is damaged, injured, or chronically inflamed. The therapy involves superficial injections of dextrose along cutaneous nerve pathways. Injections of dextrose correct glycopenia (low levels of glucose) restoring energy balance and raising pH creating a more neutral environment and restoring tissue physiology. The dextrose also opens ion-gated channels to decrease nerve signaling, which calms down the inflammation around the nerve allowing time for the nerve to heal.
- These therapies can be combined with prolotherapy to treat ligaments associated with joint instability in the low back, sacrum, and foot.
Osteoarthritis of the hip joint is degeneration of cartilage and joint space narrowing. Osteoarthritis is caused by chronic low-grade inflammatory responses from chronic overuse. Chronic inflammatory processes produce degrading enzymes trying to clean up the inflammatory debris that overtime weaken collagen networks and breakdown cartilage. Even metabolic processes such as diabetes and cardiovascular disease contribute to inflammatory responses leading to cartilage damage inside the joint. As cartilage breaks down there is abnormal bone formation (osteophytes) trying to stabilize a weakened joint, tearing of surrounding connective tissue, and loss of synovial fluid which provides nutrients and acts a shock absorber.
Common symptoms are joint pain, limited ability to sit, stand or walk, decreased range of motion, symptoms are worse in the morning and exacerbated by increased activity.
Conservative treatments are non-steroidal anti-inflammatory (NSAIDs) like ibuprofen or Advil, physical therapy, steroid injections, hyaluronic acid injection. If osteoarthritis is severe enough surgical intervention is a total hip replacement. Chronic NSAID use has been shown to lead to increased risk of stomach ulcers, acute renal failure, and stroke/myocardial infarction. Corticosteroid injections pain relief is temporary and can cause further soft tissue damage, cell death, reduced bone mineral density, and inhibit collagen synthesis.
Regenerative Medicine Treatments for Osteoarthritis of the Hip
Regenerative medicine injections stimulate the body’s natural immune response encouraging growth factors, fibroblast, immune cells, stem cells and collagen building precursors to the injured area to promote healing and repair.
- Platelet-rich plasma (PRP) therapy involves using your own blood plasma and platelets as an enriched source of growth factors, immune cells, and collagen-building precursors to stimulate healing of bone and soft tissue. PRP has been shown to modulate the repair and regeneration of damaged articular cartilage in the joints and delay further degeneration of cartilage. Studies have replicated reduction in pain, decreased inflammation in the joint space and improvement in the quality of life scores.
- Studies have found that intra-articular platelet-rich plasma injections of the hip to treat hip osteoarthritis, are well tolerated and potentially efficacious in delivering long-term and clinically significant pain reduction and functional improvement.
- Autologous stem cell (from your own body) therapies using both mesenchymal stromal cells (MSCs) and hematopoietic stem cells have shown therapeutic potential for advanced osteoarthritis. In orthopedic injuries and degeneration, stem cells have the potential to signal for the repair of damaged tissue with possible regeneration of tissue. It is important to note that research is mixed with regard to whether regenerative medicine truly regenerates tissue. What does seem to be more reproducible is a decrease in further degenerative changes, pain, and improved function.
- Platelet-rich plasma (PRP) therapy with Surgery
- “Recent studies support the use of PRP intra-articular injections, not only as a conservative treatment, but also after surgical procedures as many researchers attempted to enhance cartilage repair by combining surgical procedures such as microfractures with growth factors (GFs). PRP has been shown to improve the reparative response of focal defects of articular cartilage after surgery compared to surgery alone and also to increase the durability of repair tissue over time”
- doi:10.11138/ccmbm/2013.10.1.026
- “Recent studies support the use of PRP intra-articular injections, not only as a conservative treatment, but also after surgical procedures as many researchers attempted to enhance cartilage repair by combining surgical procedures such as microfractures with growth factors (GFs). PRP has been shown to improve the reparative response of focal defects of articular cartilage after surgery compared to surgery alone and also to increase the durability of repair tissue over time”
Regenerative Medicine does not work for everyone and there are many variables to be considered when choosing what treatment is right for you. Differences in PRP concentrations, PRP preparation methods, source of stem cells, injection techniques, accurate diagnosis, determination of pain generators, conjunction with other therapies from everything to different injection therapies to physical therapy.
It should not be underestimated the importance of treating whole-body inflammation and optimizing immune function in order to get the best results from treatments. All of these should be considered and I believe comprehensive treatments lead to optimal healing.
Research Studies and References
The Use of Ultrasound-Guided Platelet-Rich Plasma Injections in the Treatment of Hip Osteoarthritis: A Systematic Review of the Literature
- Ali M, Mohamed A, Ahmed HE, Malviya A, Atchia I. The use of ultrasound-guided platelet-rich plasma injections in the treatment of hip osteoarthritis: a systematic review of the literature. J Ultrason. 2018;18(75):332–337. doi:10.15557/JoU.2018.0048
- Purpose: This review aims to determine whether ultrasound-guided platelet-rich plasma injection has any role in improving clinical outcomes in patients with hip osteoarthritis.
- Conclusions: Literature to date concludes that intra-articular platelet-rich plasma injections of the hip, performed under ultrasound guidance to treat hip osteoarthritis, are well tolerated and potentially efficacious in delivering long-term and clinically significant pain reduction and functional improvement in patients with hip osteoarthritis. Larger future trials including a placebo group are required to further evaluate these promising results.
Different Intra-articular Injections as Therapy for Hip Osteoarthritis: A Systematic Review and Network Meta-analysis
- Zhao Z, Ma JX, Ma XL. Different Intra-articular Injections as Therapy for Hip Osteoarthritis: A Systematic Review and Network Meta-analysis [published online ahead of print, 2020 Jan 6]. Arthroscopy. 2020;S0749-8063(19)30885-0. doi:10.1016/j.arthro.2019.09.043
- Purpose: This systematic review evaluated 11 randomized controlled trials with a total of 1,060 patients to compare the clinical outcomes between 4 intra-articular injections (platelet-rich plasma [PRP], hyaluronic acid [HA], corticosteroid [CS], and HA plus PRP) for hip osteoarthritis (OA).
- Conclusion: Corticosteroid injections are recommended as the most efficient agent in hip OA patients in the short term. Moreover, PRP is reported to have the highest rank for pain relief for up to 6 months. PRP are the most efficient for pain reduction in the long term.
PRP for Degenerative Cartilage Disease: A Systematic Review of Clinical Studies
- Laver L, Marom N, Dnyanesh L, Mei-Dan O, Espregueira-Mendes J, Gobbi A. PRP for Degenerative Cartilage Disease: A Systematic Review of Clinical Studies. Cartilage. 2017;8(4):341–364. doi:10.1177/1947603516670709
- Objective: To explore the utilization of platelet-rich plasma (PRP) for degenerative cartilage processes and evaluate whether there is sufficient evidence to better define its potential effects. Twenty-six studies examined PRP administration for knee OA and 3 involved PRP administration for hip OA.
- Conclusion: Current clinical evidence supports the benefit in PRP treatment for knee and hip OA, proven to temporarily relieve pain and improve function of the involved joint with superior results compared with several alternative treatments. Further research to establish the optimal preparation protocol and characteristics of PRP injections for OA is needed.
Rheumatoid Arthritis is an autoimmune disorder that affects synovial membranes and articular surfaces in the joint space. Rheumatoid arthritis can occur in any joint in the body. It often is noticed in smaller joints first such as fingers and toes though it may affect multiple joints at once. Individuals will experience morning stiffness, pain and stiffness is usually on both sides, fatigue, weakness, and joint swelling are common.
The common etiology of all autoimmune disorders is chronic inflammation. This results in an overwhelmed immune system, which leads to immune dysfunction and the inability of the body’s defense system to recognize self from non-self.
This means your body starts seeing its own tissues as foreign and attacks the tissues like they are the common cold virus. This results in even more inflammation, and your body becomes stuck in a vicious dysfunctional cycle.
Current conventional treatments focus on symptom suppression using nonsteroidal anti-inflammatory drugs, steroids, or immune-modulating drugs. The problem with these pharmaceutical treatments is they severely depress an already depressed immune system. This results in unpleasant and often debilitating side effects including, but not limited to, infections, blood sugar dysregulation, weight gain, nausea, vomiting, dizziness, gastrointestinal dysfunction, muscle pain, and fatigue. Despite this long list of side effects, people may experience only moderate relief from their symptoms or may often experience no relief at all.
There are many multifactorial causes of inflammation in the body including:
- Environmental triggers
- Dietary influences
- Intestinal permeability
- Social/psychological stressors
- Infections
- Hormonal imbalances
- Genetic susceptibility
By understanding the impact, they each have on our body we can successfully integrative a treatment approach which restores your body’s natural balance and its innate ability to heal itself.
Femoroacetabular Impingement is caused by repetitive microtrauma from an impingement of the head of the thigh bone (femoral head) against the hip socket of the pelvis (acetabulum). Femoroacetabular Impingement leads to degeneration of the labrum (a ring of fibrous cartilage that lines the hip socket) and the cartilage of the hip joint which will further lead to osteoarthritis and abnormal bone growth further exacerbating symptoms.
The progression of femoroacetabular impingement to further degenerative changes of the joint is often ligamentous instability from the repetitive microtrauma of impingement creating a harsh inflammatory environment. As instability continues the inflammatory response continues leading to a degeneration of cartilage and joint space narrowing. The body will try to stabilize the joint with bone by increasing calcium deposits leading to bone spurs, the bones rub together creating friction and further inflammatory responses and degeneration.
Common symptoms include hip and groin pain, increased pain with weight-bearing, pain with walking uphill, jumping, squatting, and sitting.
Treatment depending on severity starts conservatively with anti-inflammatories, muscle strengthening to relieve hip joint stress, non-loading activities such as cycling or elliptical.
Surgical treatment may be very helpful for cleaning out debris in the joint as well as reshaping the bone so it does not continue to impinge. A full hip replacement may be indicated depending on severity and age.
Treatment Considerations
- Surgery can significantly improve pain and mobility and should be considered in the treatment of femoroacetabular impingement. Though surgery may be the best option especially if bone growth is inhibiting range of motion. In a study to determine the incidence of osteoarthritis after arthroscopic hip surgery for Femoroacetabular Impingement Syndrome. A clinical diagnosis of hip osteoarthritis was found in approximately 22% of young patients undergoing hip arthroscopy in as little as 2 years. (1)
- Hip femoroacetabular impingement (FAI) has been found to be the primary cause of revision surgery after hip arthroscopy. Meaning that after a hip surgery using a small camera with small incisions (arthroscopy) individuals needed another surgery because they now had FAI. (4)
- Physical therapy has been shown to be efficacious in the treatment of femoroacetabular impingement and may even prevent the need for surgery. (2)
- Imaging may not tell the whole story. It is important that you are treated as an individual based on clinical history and physical exam and not just on imaging results. Radiographic signs of Femoroacetabular impingement were not associated with the degree of hip pain or a positive anterior impingement sign, which suggests that radiographic findings may not be important in the clinical diagnosis of FAI. (3)
- Stem cells are undergoing more research and have shown promising results. A study was conducted looking at the combination of hip arthroscopy and adjuvant intra-articular injections of expanded BM-MSCs (bone marrow – mesenchymal stem cells) seems to be safe and produce interesting results at middle-term follow-up in patients with large chondral defects or mild osteoarthrosis of the hip which are still not candidates or refuse a total hip replacement. (5)
- Prolotherapy and Platelet Rich Plasma (PRP) can be used for joint stability and degenerative changes in the joint space.
- Prolotherapy injections is a great therapy to help strengthen tendons and ligaments to improve joint stability. This therapy can be combined with physical therapy for further strengthening of surrounding muscles and appropriate ergonomics.
- Platelet Rich Plasma therapy involves using your own blood plasma and platelets as an enriched source of growth factors, immune cells to stimulate healing of bone and soft tissue. PRP has been shown to modulate the repair and regeneration of damaged connective tissue and delay further degeneration of connective tissue. PRP is a great therapy for partial tears and moderate arthritis.
Research Studies and References
- Rhon DI, Greenlee TA, Sissel CD, Reiman MP. The two-year incidence of hip osteoarthritis after arthroscopic hip surgery for femoroacetabular impingement syndrome. BMC Musculoskelet Disord. 2019;20(1):266. Published 2019 Jun 1. doi:10.1186/s12891-019-2646-5
- Narveson JR, Haberl MD, Nathan Vannatta C, Rhon DI. CONSERVATIVE TREATMENT CONTINUUM FOR MANAGING FEMOROACETABULAR IMPINGEMENT SYNDROME AND ACETABULAR LABRAL TEARS IN SURGICAL CANDIDATES: A CASE SERIES. Int J Sports Phys Ther. 2018;13(6):1032–1048.
- Yamauchi R, Inoue R, Chiba D, et al. Association of clinical and radiographic signs of femoroacetabular impingement in the general population. J Orthop Sci. 2017;22(1):94–98. doi:10.1016/j.jos.2016.09.014
- Lubowitz JH. Editorial Commentary: Hip Femoroacetabular Impingement Surgery Requires Improved Radiologic Research and Expert Understanding of Hip Clinical Examination. Arthroscopy. 2015;31(7):1391. doi:10.1016/j.arthro.2015.04.103
- Mardones R, Via AG, Jofré C, et al. Cell therapy for cartilage defects of the hip. Muscles Ligaments Tendons J. 2016;6(3):361–366. Published 2016 Dec 21. doi:10.11138/mltj/2016.6.3.361
The labrum is a strong fibrous cartilage rim that deepens the hip socket and allows support for the hip joint.
Tears to the labrum can be from:
- Trauma due to extreme hip rotation such as in sports like hockey, soccer, gymnastics, and dance
- Common in individuals with hypermobile joints.
- Often associated with degenerative changes in the hip.
Degenerative changes are a result of chronic low-grade inflammatory responses from overuse. Chronic inflammatory responses produce degrading enzymes trying to clean up the inflammatory debris that overtime weaken collagen networks and breakdown cartilage predisposing the weakened cartilage to tear. Labral tears in the hip associated with degenerative changes are extremely common as we age and can be asymptomatic.
Common symptoms are hip pain in the front of the hip or groin. Pain may be associated with clicking, snapping, or locking.
Treatments include activity modification, anti-inflammatory medication (NSAIDs), and steroid injections. Therapies should be carefully considered due to chronic NSAID use being shown to lead to increased risk of stomach ulcers, acute renal failure, and stroke/myocardial infarction. Corticosteroid injections pain relief is temporary and can cause further soft tissue damage, cell death, reduced bone mineral density, and inhibit collagen synthesis.
Surgical repair may be indicated depending on the severity of the tear, associated degenerative changes, and age of the individual. Surgical repair can have positive clinical outcomes; however, it should be considered there is a strong potential progression of degenerative changes following labral repair or surgery to clean up the joint (arthroscopy). The degenerative changes from these surgeries can lead to needing a joint replacement or may lead to the need for revision surgery.
- A study examining 552 arthroscopic hip procedures for symptomatic labral tears found that 20 years post arthroscopic labral debridement (removal of torn or weakened portions of the labrum) 40% needed a total hip replacement. Common factors that increased conversation to a total hip replacement were those older than 40 years old and had the presence of combined femoral head and acetabular chondral damage. the probability of conversion to total hip replacement by 20 years post labral tear repair and arthroscopy from 12% for a patient younger than 40 years with a Grade 0-II femoral and acetabular Outerbridge grade to 92% (for a patient older than 40 years with a Grade III-IV femoral and acetabular Outerbridge grade. (2)
- In research done at Physical Medicine & Rehabilitation, Mount Sinai Hospital, New York they determined the importance of the evidence supporting the acetabular labrum’s role in preventing premature arthritis and enhancing stability of the hip joint. They found that when conservative measures fail, surgery is necessary and the philosophy behind this has shifted, now that there is evidence supporting the acetabular labrum’s role in preventing premature arthritis. Success rates of arthroscopic labral debridement (removal of torn or weakened portions of the labrum) are lower with worsening degrees of labral tear and secondary degenerative (osteoarthritis) changes. With these findings, they concluded that surgeons’ arthroscopic debridement of labral tears should be done to preserve as much healthy labral tissue as possible to stabilize the joint and prevent early-onset osteoarthritis (3)
Based on these findings regenerative medicine is an extremely important treatment for labral tears especially when there are degenerative changes in the hip joint.
- Platelet Rich Plasma therapy involves using your own blood plasma and platelets as an enriched source of growth factors, immune cells to stimulate healing of bone and soft tissue. PRP has been shown to modulate the repair and regeneration of damaged connective tissue and delay further degeneration of connective tissue. PRP is a great therapy for partial tears and moderate arthritis.
- PRP has shown promise as a minimally invasive treatment for hip labral tears. Studies have shown decreased pain and improved function with treatments.
- PRP injections can help not only in cases of osteoarthritis but also with high-level athletes who present with acute hip inflammation due to intra-articular pathology such as femoroacetabular impingement-induced labral tear. In these cases, PRP improves inflammatory symptoms and enables a quick return to play without the possible negative effects of steroids. (1)
- Autologous stem cell (from your own body) therapies using both mesenchymal stromal cells (MSCs) and hematopoietic stem cells have shown therapeutic potential for advanced osteoarthritis. In orthopedic injuries and degeneration, stem cells have the potential to signal for the repair of damaged tissue with possible regeneration of tissue. It is important to note that research is mixed with regard to whether regenerative medicine truly regenerates tissue. What does seem to be more reproducible is a decrease in further degenerative changes, pain, and improved function.
Research Studies and References
- Kraeutler MJ, Garabekyan T, Mei-Dan O. The use of platelet-rich plasma to augment conservative and surgical treatment of hip and pelvic disorders. Muscles Ligaments Tendons J. 2016;6(3):410–419. Published 2016 Dec 21. doi:10.11138/mltj/2016.6.3.410
- Dwyer MK, Tumpowsky C, Boone A, Lee J, McCarthy JC. What Is the Association Between Articular Cartilage Damage and Subsequent THA 20 Years After Hip Arthroscopy for Labral Tears?. Clin Orthop Relat Res. 2019;477(5):1211–1220. doi:10.1097/CORR.0000000000000717
- Groh MM, Herrera J. A comprehensive review of hip labral tears. Curr Rev Musculoskelet Med. 2009;2(2):105–117. doi:10.1007/s12178-009-9052-9
Use of Platelet-Rich Plasma for the Treatment of Acetabular Labral Tear of the Hip: A Pilot Study
- De Luigi AJ, Blatz D, Karam C, Gustin Z, Gordon AH. Use of Platelet-Rich Plasma for the Treatment of Acetabular Labral Tear of the Hip: A Pilot Study. Am J Phys Med Rehabil. 2019;98(11):1010–1017. doi:10.1097/PHM.0000000000001237
- Objective: This study aims to assess whether ultrasound-guided injection of platelet-rich plasma can safely and effectively treat symptoms associated with acetabular hip labral tears.
- Conclusions: Ultrasound-guided injection of platelet-rich plasma holds promise as an emerging, minimally invasive technique toward symptom relief, reducing pain, and improving function in patients with hip labral tears.
Ultrasound-Guided Injection of Platelet-Rich Plasma and Hyaluronic Acid, Separately and in Combination, for Hip Osteoarthritis: A Randomized Controlled Study
- Dallari D, Stagni C, Rani N, et al. Ultrasound-Guided Injection of Platelet-Rich Plasma and Hyaluronic Acid, Separately and in Combination, for Hip Osteoarthritis: A Randomized Controlled Study. Am J Sports Med. 2016;44(3):664–671. doi:10.1177/0363546515620383
- Background: The effectiveness of intra-articular platelet-rich plasma (PRP) injections has been evaluated in knee chondroplasty and osteoarthritis (OA); however, little evidence of its efficacy in hip OA exists.
- Conclusion: Results indicated that intra-articular PRP injections offer a significant clinical improvement in patients with hip OA without relevant side effects. The benefit was significantly more stable up to 12 months as compared with the other tested treatments. The addition of PRP+HA did not lead to a significant improvement in pain symptoms.
Avascular Necrosis or Osteonecrosis is a result of decreased blood supply to the head of the thigh bone (femur), which sits in the socket of the pelvis. Without a blood supply, the bone is unable to get nourishment and dies (necrosis). Causes of disruption of blood supply can be from trauma such as fracture or dislocation, corticosteroid use, alcohol abuse, or blood disorders.
Common symptoms are hip, groin, or gluteal pain that may refer to the thigh or knee. Decreased range of motion with a catching or popping sensation.\
Treatment Options
- Avascular Necrosis grade I and II may respond to platelet-rich plasma and autologous stem cell treatments with stem cell sources from both adipose and bone marrow. Using both adipose and bone marrow allows for mesenchymal stem cells, which signal the body’s regenerative and healing mechanisms and hematopoietic stem cells, which signal for increased blood supply to the area. This is important because avascular necrosis is due to a lack of blood supply resulting in bone death.
- Surgical intervention at this stage would be core decompression involving drilling into the area of dead bone to reduce pressure and increase blood flow.
- A study cited below found a complete resolution of AVN in a 43-year old man after four weekly injections with a mixture of PRP and autologous adipose-derived stem cells (ASCs) into the femoral head under US guidance
- Avascular Necrosis grade III and IV which means there has been a collapse of the bone (femur head) usually requires an arthroplasty or full hip replacement.
Research Studies and References
Complete Resolution of Avascular Necrosis of the Human Femoral Head Treated With Adipose Tissue-Derived Stem Cells and Platelet-Rich Plasma
- Pak J, Lee JH, Jeon JH, Lee SH. Complete resolution of avascular necrosis of the human femoral head treated with adipose tissue-derived stem cells and platelet-rich plasma. J Int Med Res. 2014;42(6):1353–1362. doi:10.1177/0300060514546940
- Objective: To determine if treatment avascular necrosis (AVN) grade I of the femoral head treated with adipose tissue-derived stem cells (ASCs) and platelet-rich plasma (PRP) was effective.
- Conclusion: The patient’s severe hip pain was considerably improved at 3 months after treatment, with pain scores, range of motion and MRI showing near complete resolution of AVN. Pain scores, ROM and MRI at 18 and 21 months after treatment indicated complete resolution of AVN.
Arthroscopic Management and Platelet-Rich Plasma Therapy for Avascular Necrosis of the Hip
- Guadilla J, Fiz N, Andia I, Sánchez M. Arthroscopic management and platelet-rich plasma therapy for avascular necrosis of the hip. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):393–398. doi:10.1007/s00167-011-1587-9
- Purpose: The purpose is to describe a noninvasive arthroscopic procedure as an alternative to open surgery for avascular necrosis of the hip. Patients with grade I or IIA avascular necrosis of the hip are treated by core decompression performed by drilling under fluoroscopic guidance and platelet-rich plasma (PRP)
- Conclusions: Arthroscopic management of avascular necrosis of the femoral head is viable and has significant advantages. Clinical studies should justify the theoretical additional benefits of this approach using platelet rich plasma. Patients with grade I or IIA AVN of the femoral head, all patients had complete resolution of pain and resolution of the lesion on follow-up MRI.
I am so grateful to Dr. Squires for healing my whiplash injury and my gut. I had intensive chronic (daily) pain from a car accident in 2004. I went to many massage practitioners, chiropractors, and acupuncturists for help, but my pain was not noticeably or sustainably reduced until I began working with Dr. Squires.
