Natural Knee Pain Relief
Knee pain is incredibly common and affects millions of individuals. Knee pain is commonly a result of the aging process, continual wear and stress on the knee joint results in degenerative changes or arthritis. Knee pain can also be a result of an injury such as sudden movement that strains the knee during sports or recreational activities.
The knee is a key weight-bearing joint with a complex structure reinforced by fibrocartilage, multiple ligaments, and tendons that provide structure and support. Despite strong reinforcement and the ability to perform in so many positions, the knee is vulnerable to both direct injury and chronic low-grade wear and tear.
Whether an individual’s knee pain is caused by aging or injury, it can be both inhibitory and debilitating. Depending on the levels of degeneration or severity of injury regenerative medicine may be an efficacious treatment to promote regeneration and repair when surgery is not indicated.
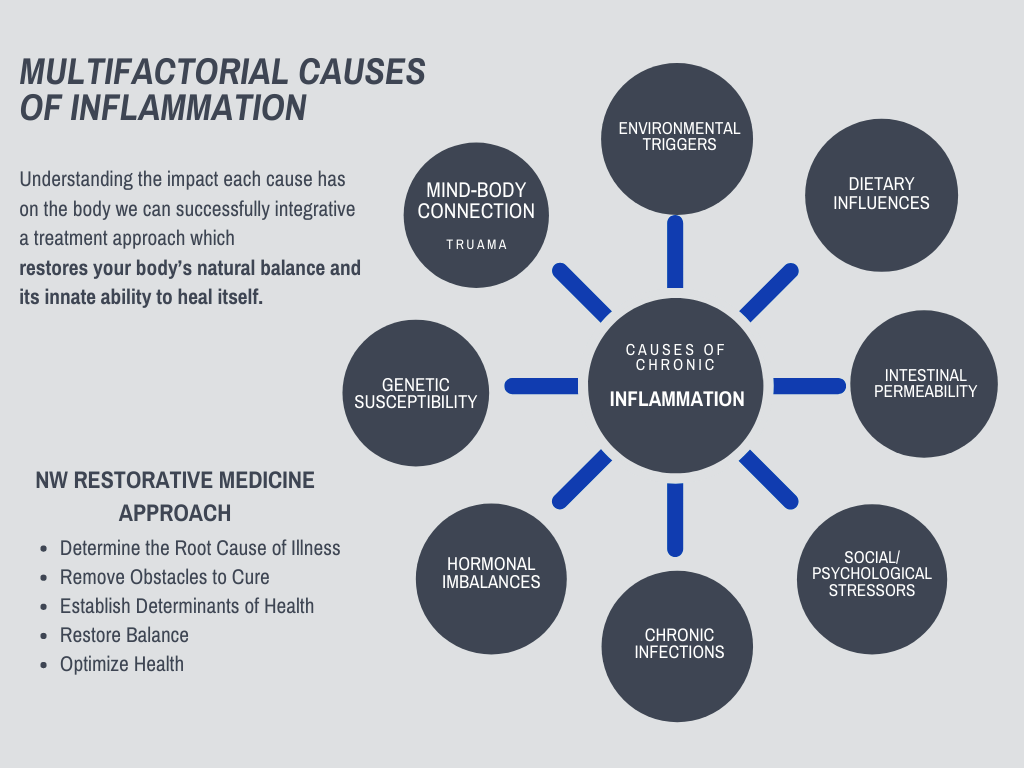
Your Knee is Connected to Your Whole Body, and so is Your Pain and Inflammation
As a result, the cause of knee pain and inflammation comes from many factors, requiring a whole-body approach to relieving pain.
Dr. Squires’ approach brings together a holistic treatment of all the factors contributing to your chronic inflammation and pain. Personalizing treatment to the factors most impacting your source of pain.
And combines it with a Regenerative Medicine approach that stimulates your own body’s healing response naturally.
Regenerative medicine is a cell-based therapy using advanced scientific techniques in the treatment of degenerative disease, orthopedic injuries, and joint conditions.
Discover how Dr. Squires can help by scheduling an initial consult »
Common Knee Problems Resulting in Pain:
Arthritis/Degenerative Changes
Patellar Tendonitis/Tendinosis
Patellofemoral Pain Syndrome and Chondromalacia Patella
Medial Collateral Ligament (MCL) Sprains/Tears
Lateral Collateral Ligament (LCL) and Posterior Corner Injuries
Anterior Cruciate Ligament (ACL) Injuries
The most common cause of knee pain is osteoarthritis. This can be a gradual process of destruction of the cartilage and articular surfaces of the knee from chronic microtrauma thought of as wear or tear. It can also be a result of previous trauma that never fully healed, congenital deformity or continual misalignments, infections, or metabolic disorders.
A way to think about the root cause of osteoarthritis is to think about ligamentous instability from a trauma/injury or overuse. Instability of a joint results in chronic inflammatory responses leading to degeneration of cartilage and joint space narrowing. If healing does not occur as the injury or instability continue our bodies will continue compensating by increasing calcium deposits leading to bone spurs, further inflammatory responses, and degeneration.
Current treatments for knee pain and osteoarthritis are bracing, weight loss, non-steroidal anti-inflammatories (NSAIDs) such as ibuprofen/Advil, corticosteroids, and surgery.
Though these options have their place, unfortunately, they all have vast limitations and/or severe side effects. A knee replacement on average lasts 15 years, which is why they are prolonged for as long as possible resulting in people resorting to chronic NSAID and corticosteroid use for pain management. Research shows that corticosteroids lead to soft tissue damage, cell death, tendon atrophy, and inhibit collagen synthesis. Chronic non-steroidal anti-inflammatories use has been shown to lead to increased risk of stomach ulcers and can be toxic to the kidneys and liver.
Regenerative Medicine for Osteoarthritis
- Platelet-rich plasma (PRP) therapy involves using your own blood plasma and platelets as an enriched source of growth factors, immune cells, and collagen-building precursors to reduce inflammation and stimulate healing of bone and soft tissue. PRP has been shown in studies to be more effective than hyaluronic acid and corticosteroids in reducing pain and improving function.
- Autologous stem cell (from your own body) therapies using both mesenchymal stromal cells (MSCs) and hematopoietic stem cells has shown therapeutic potential for advanced osteoarthritis. In orthopedic injuries and degeneration, stem cells have the potential to signal for the repair of damaged tissue with possible regeneration of tissue. It is important to note that research is mixed with regard to whether regenerative medicine truly regenerates tissue. What does seem to be more reproducible are a decrease in further degenerative changes, pain, and improved function.
Regenerative Medicine does not work for everyone and there are many variables to be considered when choosing what treatment is right for you. Differences in PRP concentrations, PRP preparation methods, source of stem cells, injection techniques, accurate diagnosis, determination of pain generators, conjunction with other therapies from everything to different injection therapies to physical therapy.
It should not be underestimated the importance of treating whole-body inflammation and optimizing immune function in order to get the best results from treatments. All of these should be considered and I believe comprehensive treatments lead to optimal healing.
Research Studies and References
“The therapeutic potential of mesenchymal stromal cells (MSCs) is evident by the number of new and ongoing trials targeting an impressive variety of conditions.”
- Heldring N, Mäger I, Wood MJ, Le Blanc K, Andaloussi SE. Therapeutic Potential of Multipotent Mesenchymal Stromal Cells and Their Extracellular Vesicles. Hum Gene Ther. 2015;26(8):506–517. doi:10.1089/hum.2015.072
The University of California published mechanisms for how PRP modulates the repair and regeneration of joint tissue in osteoarthritis in the journal Tissue engineering. Part B, Platelet-Rich Plasma Modulates Actions on Articular Cartilage Lubrication and Regeneration.
- Sakata R, Reddi AH. Platelet-Rich Plasma Modulates Actions on Articular Cartilage Lubrication and Regeneration. Tissue Eng Part B Rev. 2016 Apr 25
- PRP modulates the repair and regeneration of damaged articular cartilage in the joints and delays the degeneration of cartilage by stimulation of mesenchymal stem cell migration, proliferation, and differentiation into articular chondrocytes (the cells of cartilage).
- PRP has the therapeutic potential not only to promote tissue regeneration, but also to contribute to articular cartilage lubrication by decreasing the friction coefficient and minimizing wear
- They also determined the reduction of pain is a result of decreased inflammation of the synovial membrane where pain receptors are located
In a systematic review published in the journal of Arthroscopy: The Journal of Arthroscopic & Related Surgery, Efficacy of Intra-articular Platelet-Rich Plasma Injections in Knee Osteoarthritis: A Systematic Review. Six studies comparing the efficacy of hyaluronic acid and PRP treatments for symptomatic osteoarthritis were reviewed (739 patients, 817 knees, 39% males with a mean age of 59.9 years)
- Meheux CJ, McCulloch PC, Lintner DM, Varner KE, Harris JD. Efficacy of Intra-articular Platelet-Rich Plasma Injections in Knee Osteoarthritis: A Systematic Review. Arthroscopy. 2015 Sep 29. pii: S0749-8063(15)00659-3. doi: 10.1016/j.arthro.2015.08.005
- Purpose: To determine (1) whether platelet-rich plasma (PRP) injection significantly improves validated patient-reported outcomes in patients with symptomatic knee osteoarthritis (OA) at 6 and 12 months postinjection, (2) differences in outcomes between PRP and corticosteroid injections or viscosupplementation or placebo injections at 6 and 12 months postinjection, and (3) similarities and differences in outcomes based on the PRP formulations used in the analyzed studies.
- Conclusions: In patients with symptomatic knee OA, PRP injection results in significant clinical improvements up to 12 months postinjection. Clinical outcomes and WOMAC scores are significantly better after PRP versus HA at 3 to 12 months postinjection. There is limited evidence for comparing leukocyte-rich versus leukocyte-poor PRP or PRP versus steroids in this study.
In study published in Sports Med Phys Fitness, Effect of single injection of platelet-rich plasma in comparison with corticosteroid on knee osteoarthritis: a double-blind randomized clinical trial compared PRP injections to cortisone steroid injections in the treatment of osteoarthritis.
In the study 41 participants were randomly divided and given either a PRP or cortisone injection.
- Forogh B, Mianehsaz E, Shoaee S, Ahadi T, Raissi GR, Sajadi S. Effect of single injection of Platelet-Rich Plasma in comparison with corticosteroid on knee osteoarthritis: a double-blind randomized clinical trial. J Sports Med Phys Fitness. 2015 Jul 14.
- Purpose: Comparison of platelet-rich plasma with corticosteroids on knee arthritis.
- Conclusions: Our study demonstrated that one shot of PRP injection, decreased joint pain more and longer-term, alleviated the symptoms, and enhanced the activity of daily living and quality of life in short-term duration in comparison with corticosteroids.
- Results showed that the PRP group compared to the group treated with corticosteroid injection had improved pain relief based on the VAS (visual analog scale), improved activities of daily living and quality of life at 2 and 6 month follow ups. PRP also was more helpful in improving the 20 meter walk test than corticosteroid treatment, however none of the treatments had any impact on active or passive range of motion.
Bone Marrow Aspirate Concentrate for the Treatment of Knee Osteoarthritis: A Systematic Review
- Keeling LE, Belk JW, Kraeutler MJ, Kallner AC, Lindsay A, McCarty EC, Postma WF. Bone Marrow Aspirate Concentrate for the Treatment of Knee Osteoarthritis: A Systematic Review. Am J Sports Med. 2021 Jul 8:3635465211018837. doi: 10.1177/03635465211018837. Epub ahead of print. PMID: 34236913.
- Purpose: To systematically review the literature to evaluate the efficacy of isolated BMAC injection in the treatment of OA of the knee joint.
- Conclusion: The BMAC injection is effective in improving pain and patient-reported outcomes in patients with knee OA at short- to midterm follow-up. Nevertheless, BMAC has not demonstrated clinical superiority in relation to other biologic therapies commonly used in the treatment of OA, including platelet-rich plasma and microfragmented adipose tissue, or in relation to placebo. The high cost of the BMAC injection in comparison with other biologic and nonoperative treatment modalities may limit its utility despite demonstrable clinical benefit.
Inflammation of patellar tendon secondary to repetitive trauma often referred to as “jumper’s knee”. This is a common injury in sports like basketball, tennis, or volleyball, but will happen with running and cycling as well. Patellar tendinosis/tendinitis results in tenderness and pain below the knee cap that worsens with activity. Conservative treatments such as rest, ice, and anti-inflammatories may help though it is important to note that steroid injections should not be used due to the increased risk of tendon rupture.
As you can see in the studies below regenerative medicine injections and shockwave therapy are efficacious treatment options.
In summary, tendinopathies are due to overuse and trauma, caused by inflammation, degeneration, and weakening of the tendon, which may eventually lead to tendon rupture.
- Tendon healing can be stimulated by regenerative medicine therapies through a dynamic process of inflammatory cascades, cellular proliferation, and tissue remodeling.
- Regenerative medicine injections recruit the body’s natural immune cells and inflammatory response, promoting growth factors and collagen-building precursors to the injured area to promote healing, remodeling, and repair.
Research Studies and References
Use of platelet-rich plasma for the treatment of refractory jumper’s knee
- Filardo G, Kon E, Della Villa S, Vincentelli F, Fornasari PM, Marcacci M. Use of platelet-rich plasma for the treatment of refractory jumper’s knee. Int Orthop. 2010;34(6):909–915. doi:10.1007/s00264-009-0845-7
- Purpose: The aim of this study was to evaluate the efficacy of multiple platelet-rich plasma (PRP) injections on the healing of chronic refractory patellar tendinopathy after previous classical treatments have failed.
- Conclusions: A statistically significant improvement in all scores was observed at the end of the PRP injections in patients with chronic refractory patellar tendinopathy and a further improvement was noted at six months, after physiotherapy was added. The clinical results are encouraging, indicating that PRP injections have the potential to promote the achievement of a satisfactory clinical outcome, even in difficult cases with chronic refractory tendinopathy after previous classical treatments have failed.
Pain and activity levels before and after platelet-rich plasma injection treatment of patellar tendinopathy: a prospective cohort study and the influence of previous treatments.
- Gosens T, Den Oudsten BL, Fievez E, van ‘t Spijker P, Fievez A. Pain and activity levels before and after platelet-rich plasma injection treatment of patellar tendinopathy: a prospective cohort study and the influence of previous treatments. Int Orthop. 2012;36(9):1941–1946. doi:10.1007/s00264-012-1540-7
- Purpose: The aim of this study was to evaluate the outcome of patients with patellar tendinopathy treated with platelet-rich plasma injections (PRP).
- Conclusion: After PRP treatment, patients with patellar tendinopathy showed a statistically significant improvement. In addition, these improvements can also be considered clinically meaningful.
Treatment Options for Patellar Tendinopathy: A Systematic Review
- Everhart JS, Cole D, Sojka JH, et al. Treatment Options for Patellar Tendinopathy: A Systematic Review. Arthroscopy. 2017;33(4):861–872. doi:10.1016/j.arthro.2016.11.007
- Purpose: To compare the efficacy of common invasive and noninvasive patellar tendinopathy (PT) treatment strategies.
- Conclusions: Initial treatment of PT can consist of eccentric squat-based therapy, shockwave, or PRP as monotherapy or an adjunct to accelerate recovery. Surgery or shockwave can be considered for patients who fail to improve after 6 months of conservative treatment. Corticosteroid therapy should not be used in the treatment of PT.
The effectiveness of extracorporeal shock wave therapy in lower limb tendinopathy: a systematic review
- Mani-Babu S, Morrissey D, Waugh C, Screen H, Barton C. The effectiveness of extracorporeal shock wave therapy in lower limb tendinopathy: a systematic review. Am J Sports Med. 2015;43(3):752–761. doi:10.1177/0363546514531911
- Purpose: To evaluate the effectiveness of ESWT for lower limb tendinopathies.
- Conclusion: Extracorporeal shock wave therapy is an effective intervention and should be considered for greater trochanteric pain syndrome (GTPS), patellar tendinopathy (PT), and Achilles tendinopathy (AT) particularly when other nonoperative treatments have failed.
Platelet-rich Plasma Versus Focused Shock Waves in the Treatment of Jumper’s Knee in Athletes
- Vetrano M, Castorina A, Vulpiani MC, Baldini R, Pavan A, Ferretti A. Platelet-rich plasma versus focused shock waves in the treatment of jumper’s knee in athletes. Am J Sports Med. 2013;41(4):795–803. doi:10.1177/0363546513475345
- Purpose: To compare the effectiveness and safety of platelet-rich plasma (PRP) injections and focused extracorporeal shock wave therapy (ESWT) in athletes with jumper’s knee.
- Conclusion: Therapeutic injections of PRP lead to better midterm clinical results at 6 and 12 month follow up compared with focused ESWT in the treatment of jumper’s knee in athletes.
Comparing PRP Injections With ESWT for Athletes With Chronic Patellar Tendinopathy
- Smith J, Sellon JL. Comparing PRP injections with ESWT for athletes with chronic patellar tendinopathy. Clin J Sport Med. 2014;24(1):88–89. doi:10.1097/JSM.0000000000000063
- Purpose: To compare the effectiveness of injections of platelet-rich plasma (PRP) compared with focused extracorporeal shock-wave therapy (ESWT) among athletes with chronic patellar tendinopathy (jumper’s knee).
- Conclusions: Athletes with chronic patellar tendinopathy responded positively to both PRP injection and ESWT. However, the PRP-treated patients demonstrated significantly greater improvements in VISA-P and pain scores by 6 months and significantly better functional outcomes and satisfaction based on a modified Blazina scale, at 12 months.
Patellofemoral Pain Syndrome (PFPS) is the most common type of kneecap pain often referred to as “runner’s knee”. PFPS occurs when the kneecap does not stay in the patellar groove and can move off to the side creating discomfort when using stairs, running, standing from sitting, or doing squats. The cause of the PFPS is a combination of overuse, activity during misalignment, and biomechanical factors such as muscle weakness, lack of flexibility, decreased range of motion, uneven leg lengths, and ankles that roll in too much (hyper pronation) or flat feet. Chondromalacia Patellae is a condition that is associated with patellofemoral pain syndrome. Chondromalacia patellae is a softening of articular cartilage with associated degenerative changes behind the knee cap.
The pathology of these conditions is thought to be repetitive microtrauma or acute trauma such as a ligament or tendon tear that can result in chronic inflammatory responses contributing to cartilage insult and breakdown of the tissue surrounding the knee.
Management of symptoms may include physical therapy, use of non-steroidal anti-inflammatories, or topicals to reduce pain. Surgical intervention can include debridement of diseased cartilage, lateral retinacular release, and re-alignment procedures.
This is a condition that may respond well to regenerative medicine specifically Prolotherapy, platelet-rich plasma (PRP) and/or stem cell therapy depending on severity.
Research Studies and References
Effectiveness of PRP on Pain, Function and Quality of Life in Chondromalacia and Patellofemoral Pain Syndrome: A Pretest-Posttest Analysis.
- Olga Susana Pérez Moro1, María Jesús Albaladejo Florín1 et al. Effectiveness of PRP on Pain, Function and Quality of Life in Chondromalacia and Patellofemoral Pain Syndrome: A Pretest-Posttest Analysis. Research Article Volume 1 Issue 1 – May 2017 DOI: 10.19080/NTAB.2017.01.555554
- Purpose: To demonstrate the effectiveness of a 3-doses PRP treatment protocol on pain, function and quality of life (QoL) in patients with Patellofemoral Pain Syndrome (PFPS) and Chondromalacia. To apply PRP as a conservative treatment option with a demonstrable level of scientific evidence.
- Conclusion: PRP is safe and significantly improves pain relief, stiffness and function in patients with Patellofemoral Pain Syndrome and Chondromalacia.
Outcomes of Prolotherapy in Chondromalacia Patella
- Hauser, R. A., & Sprague, I. S. (2014). Outcomes of Prolotherapy in Chondromalacia Patella Patients: Improvements in Pain Level and Function. Clinical Medicine Insights: Arthritis and Musculoskeletal Disorders.
- Purpose: Evaluation of the effectiveness of prolotherapy in resolving pain, stiffness, and crepitus, and improving physical activity in consecutive chondromalacia patients.
- Conclusion: Patients experienced statistically significant decreases in pain at rest, during activities of daily living, and exercise. Stiffness and crepitus decreased after Prolotherapy, and ROM increased.
Medial collateral ligaments (MCL) injuries often happen during sports such as football when an individual is hit on the outside of the knee putting strain on the inside of the knee joint. Often these injuries include the anterior cruciate ligament and the medial meniscus. An MCL injury in isolation is usually treated with rest and functional rehabilitation. Some individuals may experience chronic persistent medial knee pain after isolated low-grade injuries of medial collateral ligaments (MCL).
These injuries despite conservative treatments may have insufficient healing of ligaments resulting in ongoing pain and dysfunction. MCL sprains grade 1, interstitial tear with no joint laxity, and grade 2, partial tear, are ideal injuries to be treated with regenerative medicine. Regenerative medicine can stimulate a healing/inflammatory response to the injured area initiating proper healing.
If the MCL injury is severe such as a complete rupture surgical repair or reconstruction may be the best option.
In summary, an MCL injury often involves other ligaments and structures. Regenerative medicine including prolotherapy, perineural injection therapy, and platelet-rich plasma would need to be comprehensive treating all injured ligaments, tendons, and nerves.
- Comprehensive regenerative medicine to the knee involves multiple injections to all of the affected ligaments and other injured structures of the knee.
- Regenerative medicine injections stimulate the body’s natural immune response, an inflammatory response, encouraging growth factors and collagen-building precursors to the injured area to promote healing and repair.
Research Studies and References
An Autologous Leukocyte-Reduced Platelet-Rich Plasma Therapy for Chronic Injury of the Medial Collateral Ligament in the Knee: A Report of 3 Successful Cases
- Yoshida M, Marumo K. An Autologous Leukocyte-Reduced Platelet-Rich Plasma Therapy for Chronic Injury of the Medial Collateral Ligament in the Knee: A Report of 3 Successful Cases. Clin J Sport Med. 2019;29(1):e4–e6. doi:10.1097/JSM.0000000000000515
- Purpose: To see if chronically symptomatic MCL injuries in 3 patients using platelet-rich plasma (PRP) injections would decrease symptoms and improve function.
- Conclusion: After PRP injections, all cases returned to their sport activities at a previous level as without symptoms, and complete healing of proximal ligaments was identified on magnetic resonance images. The outcomes indicated that PRP injections led to successful repair for chronic injuries of MCL in knees.
Lateral collateral ligament (LCL) is rarely injured in isolation and happens when there is a blow to the inside of the knee usually during sports such as football or soccer. Common injuries to the LCL often accompany injuries to other stabilizing structures. It is important for a proper exam and often imaging to determine all structures involved so that you can be treated appropriately and efficiently.
Individuals will experience pain on the outside of their knee, buckling during full extension while weight-bearing and feeling unstable. These injuries despite conservative treatments may have insufficient healing of ligaments resulting in ongoing pain and dysfunction.
LCL sprains grade 1, interstitial tear with no joint laxity, and grade 2, partial tear, are ideal injuries to be treated with regenerative medicine. Regenerative medicine can stimulate a healing/inflammatory response to the injured area initiating proper healing. If the LCL injury is severe such as a complete rupture surgical repair or reconstruction may be the best option.
In summary, an LCL injury often involves other ligaments and structures. Regenerative medicine including prolotherapy, perineural injection therapy, and platelet-rich plasma is a comprehensive treatment of all injured ligaments, tendons, and nerves.
- Comprehensive regenerative medicine to the knee involves multiple injections to all of the affected ligaments and other injured structures of the knee.
- Regenerative medicine injections stimulate the body’s natural immune response, an inflammatory response, encouraging growth factors and collagen-building precursors to the injured area to promote healing and repair.
The anterior cruciate ligament is the most commonly injured ligament in the knee. Tears are most commonly caused either by a forward movement of the tibia (the long bone beneath the knee), external rotation of the femur (long bone above the knee), or stress placed on the outside of the knee.
Common injuries leading to ACL tears happen when the foot is planted and quick pivots take places such as football, soccer, basketball and tennis and is also a common injury in downhill skiing.
Regenerative Medicine Therapies for ACL injuries
- Isolated and partial ACL tears with increase in ligament length (instability) may respond well to prolotherapy and platelet rich plasma therapies.
- However, if you are young, active or a high-level athlete than reconstructive surgery may be the best choice. Some studies have shown improved recovery with platelet rich plasma injections post-surgery. Combing surgery and regenerative medicine may improve percentages of athletes being able to return to play.
- Elderly or less active individuals may not be surgical candidates and regenerative medicine therapies should be considered to help alleviate pain, improve function and decrease degenerative changes.
- ACL trauma often effects surrounding structures. The knee ligaments, may not be torn they can still be sprained, stretched, an/or loose. If these ligaments are not treated or strengthened, chronic knee instability and a continuous, abnormal, destructive low-grade inflammatory response will continue. This is the origins of knee osteoarthritis.
- Instability and degenerative process can be treated and resolved with Prolotherapy and Platelet Rich Plasma injections.
- Regenerative medicine should also be considered when there is pain and instability after surgery and usually after failed reconstruction.
Research Studies and References
Biologic Approaches for the Treatment of Partial Tears of the Anterior Cruciate Ligament: A Current Concepts Review
- Dallo I, Chahla J, Mitchell JJ, Pascual-Garrido C, Feagin JA, LaPrade RF. Biologic Approaches for the Treatment of Partial Tears of the Anterior Cruciate Ligament: A Current Concepts Review. Orthopaedic Journal of Sports Medicine. 2017 Jan 25;5(1):2325967116681724.
- Background: Anterior cruciate ligament reconstruction (ACLR) has been established as the gold standard for treatment of complete ruptures of the anterior cruciate ligament (ACL) in active, symptomatic individuals. In contrast, treatment of partial tears of the ACL remains controversial. Biologically augmented ACL-repair techniques are expanding in an attempt to regenerate and improve healing and outcomes of both the native ACL and the reconstructed graft tissue.
- Purpose: To review the biologic treatment options for partial tears of the ACL.
- Conclusion: The potential benefits of these biological augmentation approaches for partial ACL tears are improved healing, better proprioception, and a faster return to sport and activities of daily living when compared with standard reconstruction procedures. However, long-term studies with larger cohorts of patients and with technique validation are necessary to assess the real effect of these approaches.
Long-term Effects of Dextrose Prolotherapy for Anterior Cruciate Ligament Laxity
- Reeves KD, Hassanein KM. Long-term effects of dextrose prolotherapy for anterior cruciate ligament laxity. Altern Ther Health Med. 2003;9(3):58–62.
- Purpose: Determine the 1 and 3 year efficacy of dextrose injection prolotherapy on anterior cruciate ligament (ACL) laxity. After year 1, determine patient tolerance of a stronger dextrose concentration (25% versus 10%).
- Conclusion: In patients with symptomatic anterior cruciate ligament laxity, intermittent dextrose injection resulted in clinically and statistically significant improvement in ACL laxity, pain, swelling, and knee range of motion.
Is ACL reconstruction a prerequisite for the patients having recreational sporting activities?
- Morris RC, Hulstyn MJ, Fleming BC, Owens BD, Fadale PD. Return to Play Following Anterior Cruciate Ligament Reconstruction. Clin Sports Med. 2016 Oct;35(4):655-68.
- Purpose: Whether surgical or conservative treatment is more effective in allowing patients to return to physical activity after anterior cruciate ligament (ACL) injury is controversial. We sought to compare mid-term outcome measures between isolated ACL tear patients who underwent reconstruction followed by closed kinetic chain exercises and those who underwent neuromuscular training only.
- Conclusion: No statistical difference was observed between the groups for any of the parameters evaluated, including assessment of subjective knee function, one-leg hop test, assessment of joint position sense, muscle strength, and the health profile. Our data suggest that early surgical reconstruction may not be a prerequisite to returning to recreational physical activities after injury in patients with ACL tears.
Return to High School– and College-Level Football After Anterior Cruciate Ligament Reconstruction: A Multicenter Orthopaedic Outcomes Network (MOON) Cohort Study
- McCullough KA, Phelps KD, Spindler KP, Matava MJ, Dunn WR, Parker RD; MOON Group, Reinke EK. Return to High School- and College-Level Football After Anterior Cruciate Ligament Reconstruction: A Multicenter Orthopaedic Outcomes Network (MOON) CohortStudy. Am J Sports Med. 2012 Aug 24
- Background: There is a relative paucity of data regarding the effect of anterior cruciate ligament (ACL) reconstruction on the ability of American high school and collegiate football players to return to play at the same level of competition as before their injury or to progress to play at the next level of competition.
- Purpose: (1) To identify the percentage of high school and collegiate American football players who successfully returned to play at their previous level of competition, (2) to investigate self-reported performance for those players able to return to play or reason(s) for not returning to play, and (3) to elucidate risk factors responsible for players not being able to return to play or not returning to the same level of performance.
- Conclusion: Return to play percentages for amateur American football players after ACL reconstruction are not as high as would be expected. While technical aspects of ACL reconstruction and the ensuing rehabilitation have been studied extensively, the psychological factors (primarily a fear of reinjury) influencing the ability to return to play after ACL surgery may be underestimated as a critical factor responsible for athletes not returning to play at any level of competition.
Posterior cruciate ligament (PCL) injury most commonly occurs by direct trauma impacting the front of the knee such as hitting the dashboard with a bent knee. The posterior cruciate ligament is rarely injured and when it does tear they tend to be partial tears with the potential to heal on their own.
People who have injured just their posterior cruciate ligaments are usually able to return to sports without knee stability problems. Since PCL injuries usually are injured in severe trauma they usually are not injured alone.
PCL injuries often accompany injuries to other stabilizing structures. It is important for a proper exam and often imaging to determine all structures involved so that you can be treated appropriately and efficiently.
Regenerative Medicine Therapies for PCL Injuries
- Posterior cruciate ligament injury is frequently associated with multiple ligaments. The knee ligaments, may not be torn they can still be strained, stretched, an/or loose. If these ligaments are not treated or strengthened, chronic knee instability and continuous, abnormal, destructive low-grade inflammatory responses will continue.
- This instability and the degenerative process low-grade instability causes can be treated and resolved with Prolotherapy and Platelet Rich Plasma injections either before or after surgical intervention depending on multiple factors
- Regenerative medicine treatments that stimulate ligament healing and restoration should be utilized either in combination or before surgical intervention depending on the severity of the injury.
- Regenerative medicine signals an inflammatory cascade bringing increased blood flow, immune cells, and growth factors to the area of injury promoting repair and strengthening the tissue.
Research Studies and References
Posterior Cruciate Ligament Injuries
- Schüttler KF, Ziring E, Ruchholtz S, Efe T. Verletzungen des hinteren Kreuzbands [Posterior cruciate ligament injuries] [published correction appears in Unfallchirurg. 2017 Jun;120(6):530]. Unfallchirurg. 2017;120(1):55–68. doi:10.1007/s00113-016-0292-z
- Conclusion: Meticulous classification of PCL injuries taking all stabilizing factors of the knee joint as well as the time from injury into account are essential for successful treatment of PCL injuries.
Injuries to the Posterior Cruciate Ligament and Posterolateral Instabilities of the Knee
- Wang CJ. Injuries to the posterior cruciate ligament and posterolateral instabilities of the knee. Chang Gung Med J. 2002;25(5):288–297.
- Conclusion: The significance of PCL injury has been overly simplified, and the functional disability of knees with PCL injury underestimated. Combined arthroscopic PCL reconstruction and posterolateral reconstruction achieved 64% satisfactory and 36% unsatisfactory results over an average of 32 months of follow-up.
- Complete restoration of ligament stability was noted in only 44% of knees. Meaning that 66% of individuals had some level of instability.
- Despite the fact that currently employed surgical techniques only achieve modest success in restoration of ligament stability, early surgical reconstruction in knees with combined PCL and posterolateral instabilities achieved the best clinical results and a high rate of patient satisfaction.
The meniscus consists of two discs of cartilage that provides shock absorption, cushion, and joint stability. Meniscus injuries are common and can happen during a sporting event, but can also be asymptomatic and result from degenerative change for the meniscal tissue and surrounding areas.
Meniscal tears can either lead to knee osteoarthritis or knee osteoarthritis can also lead to a meniscal tear through breakdown and a weakening of the meniscal structure.
Symptoms of a meniscal tear in the knee can include a “popping” sound, knee pain, knee catching or locking, feeling like the knee is giving. Acute injuries will usually result in significant swelling and pain. The meniscus can have different types and locations of tears, which will determine the most appropriate treatment.
The repair depends on the site and extent of the damage. The periphery of the meniscus is vascular meaning it has more blood supply. When tissue has more blood supply it is able to get immune and repair cells to the area and has a greater scope for healing. The inner portion of the meniscus is avascular meaning no blood supply which inhibits healing from injury. Healing a meniscus injury depends on having enough of a blood supply and/or growth factors at the site of the injury. Platelet-rich plasma increases blood flow, immune cells, and can growth factors that enhance the meniscus healing through cell proliferation and tissue regeneration.
Regenerative Medicine for Meniscus Injuries
- Prolotherapy injections are indicated to help strengthen tendons and ligaments to improve joint stability. This therapy can be combined with physical therapy for further strengthening of surrounding muscles and appropriate ergonomics.
- Platelet Rich Plasma therapy involves using your own blood plasma and platelets as an enriched source of growth factors, immune cells to stimulate healing of bone and soft tissue. PRP has been shown to modulate the repair and regeneration of damaged connective tissue and delay further degeneration of connective tissue. PRP is a great therapy for partial tears and moderate arthritis.
- Since the meniscus is vulnerable to repetitive injury which can predispose to osteoarthritis regenerative medicine is an ideal treatment.
- Platelet-rich plasma increases blood flow to the area of injury. This should be considered for treatment options or in collaboration with surgery in all zones of healing.
- Peptides can enhance meniscus healing through cell proliferation and tissue regeneration.
Research Studies and References
Percutaneous Injections of Platelet Rich Plasma for Treatment of Intrasubstance Meniscal Lesions
- Blanke F, Vavken P, Haenle M, von Wehren L, Pagenstert G, Majewski M. Percutaneous injections of Platelet rich plasma for treatment of intrasubstance meniscal lesions. Muscles Ligaments Tendons J. 2015;5(3):162–166. Published 2015 Oct 20. doi:10.11138/mltj/2015.5.3.162
- Purpose: management of intrasubstance meniscal lesions is still controversial. Intrasubstance meniscal lesions can lead to reduced sports activity and meniscal rupture. Physical therapy is often not satisfactory. Therefore new treatment methods are requested. Platelet Rich Plasma (PRP) has the ability to regenerate tissue; this was proved in several experimental studies. We hypothesize that percutaneous PRP injections lead to pain relief and halt of progression on MRI over 6 months in patients with grade 2 meniscal lesions.
- Conclusions: percutaneous injections of PRP have the ability to achieve pain relief and halt of progression on MRI over 6 months in patients with grade 2 meniscal lesions. Therefore it could be considered as a treatment option in patients with persisting pain.
A Novel Hypothesis: The Application of Platelet-Rich Plasma Can Promote the Clinical Healing of White-White Meniscal Tears
- Wei LC, Gao SG, Xu M, Jiang W, Tian J, Lei GH. A novel hypothesis: the application of platelet-rich plasma can promote the clinical healing of white-white meniscal tears. Med Sci Monit. 2012;18(8):HY47–HY50. doi:10.12659/msm.883254
- The white-white tears (meniscus lesion completely in the avascular zone) are without blood supply and theoretically cannot heal. It has been proven that partial or all-meniscusectomy results in an accelerated degeneration of cartilage and an increased rate of early osteoarthritis.
- Platelet-rich plasma (PRP) is a platelet concentration derived from autologous blood. In recent years, PRP has been used widely in preclinical and clinical applications for bone regeneration and wound healing. Therefore, we hypothesize that the application of platelet-rich plasma for white-white meniscal tears will be a simple and novel technique of high utility in knee surgery.
Knee Osteoarthritis After Arthroscopic Partial Meniscectomy: Prevalence and Progression of Radiographic Changes After 5 to 12 Years Compared With Contralateral Knee
- Longo UG, Ciuffreda M, Candela V, et al. Knee Osteoarthritis after Arthroscopic Partial Meniscectomy: Prevalence and Progression of Radiographic Changes after 5 to 12 Years Compared with Contralateral Knee. J Knee Surg. 2019;32(5):407–413. doi:10.1055/s-0038-1646926
- Purpose: The purpose of this study was to study the clinical and radiographic changes in the knee after arthroscopic partial meniscectomy (APM) at a long-term follow-up compared with the contralateral knee.
- Conclusion: The progression of knee OA was statistically significant, ranging from 17.2% preoperatively to 65.95% postoperatively in the medial compartment and from 17.64% preoperatively to 58.82% postoperatively in the lateral compartment.
Knee Osteoarthritis After Meniscectomy: Prevalence of Radiographic Changes After Twenty-One Years, Compared With Matched Controls
- Roos H, Laurén M, Adalberth T, Roos EM, Jonsson K, Lohmander LS. Knee osteoarthritis after meniscectomy: prevalence of radiographic changes after twenty-one years, compared with matched controls. Arthritis Rheum. 1998;41(4):687–693. doi:10.1002/1529-0131(199804)41:4<687::AID-ART16>3.0.CO;2-2
- Purpose: To study the long-term outcome of surgical removal of a meniscus in the knee with regard to radiographic signs of osteoarthritis (OA).
- Conclusion: Surgical removal of a meniscus following knee injury represents a significant risk factor for radiographic tibiofemoral OA, after 21 years. Mild degenerative radiographic changes were found in 71% of the knees, while more advanced degenerative changes were seen in 48%. Compared to the control group were mild degenerative changes were seen in18% and severe degenerative changes were seen in 7%.
Meniscal Tear in Knees Without Surgery and the Development of Radiographic Osteoarthritis Among Middle-Aged and Elderly Persons: The Multicenter Osteoarthritis Study
- Englund M, Guermazi A, Roemer FW, et al. Meniscal tear in knees without surgery and the development of radiographic osteoarthritis among middle-aged and elderly persons: The Multicenter Osteoarthritis Study. Arthritis Rheum. 2009;60(3):831–839. doi:10.1002/art.24383
- Purpose: Although partial meniscectomy is a risk factor for the development of knee osteoarthritis (OA), there is a lack of evidence that meniscal damage that is not treated with surgery would also lead to OA, suggesting that surgery itself may cause joint damage. Furthermore, meniscal damage is common. The aim of this study was to evaluate the association between meniscal damage in knees without surgery and the development of radiographic tibiofemoral OA.
- Conclusion: In knees without surgery, meniscal damage is a potent risk factor for the development of radiographic OA. These results highlight the need for better understanding, prevention, and treatment of meniscal damage.
Update on Meniscus Debridement and Resection
- Weiss WM, Johnson D. Update on meniscus debridement and resection. J Knee Surg. 2014;27(6):413–422. doi:10.1055/s-0034-1388653
- Conclusion: The decision of whether to perform meniscal debridement or repair must be made on an individual basis, and characteristics of both the patient and tear should be considered. Important patient characteristics include age, cartilage status, concomitant anterior cruciate ligament reconstruction, and compliance. The determination of which patients and meniscal tears are appropriate for meniscal debridement or repair should be made on an individual basis, in consultation with the patient, based on the factors presented.
Meniscal Repair Versus Partial Meniscectomy: A Systematic Review Comparing Reoperation Rates and Clinical Outcomes
- Paxton ES, Stock MV, Brophy RH. Meniscal repair versus partial meniscectomy: a systematic review comparing reoperation rates and clinical outcomes. Arthroscopy. 2011;27(9):1275–1288. doi:10.1016/j.arthro.2011.03.088
- Purpose: The aim of this investigation was to compare reoperation rates and clinical outcomes after meniscal repair and partial meniscectomy.
- Conclusions: Whereas meniscal repairs have a higher reoperation rate than partial meniscectomies, they are associated with better long-term outcomes. meniscal repair was associated with higher Lysholm scores, examining a patient’s knee-specific symptoms including mechanical locking, instability, pain, swelling, stair climbing, and squatting, and less radiologic degeneration than partial meniscectomy.
Platelet-Rich Plasma: Does It Decrease Meniscus Repair Failure Risk?
- Everhart, Joshua Scott et al. “Platelet-Rich Plasma: Does It Decrease Meniscus Repair Failure Risk?.” Orthopaedic Journal of Sports Medicine vol. 7,7 suppl5 2325967119S00247. 29 Jul. 2019, doi:10.1177/2325967119S00247
Bakers’ cysts usually are a result of arthritis or meniscal tear fluid created by an inflammatory cascade.
The inflammation creates fluid that goes to an otherwise collapsed space creating a pocket filled with this fluid. The cyst can be drained and will give temporary relief, but unless you address the injury or degeneration it will fill again.
In order to treat a baker’s cyst, the root cause of the inflammatory response needs to be addressed.
Regenerative medicine injections stimulate an immune response to the area of injury leading to a dynamic process with inflammation, cellular proliferation, and tissue remodeling. Baker’s cyst will usually resolve with treatment of the injury and arthritis.
I injured my shoulder and was unable to really use it for about 6 months before going to see Dr. Carley Squires. She recommended Platelet-Rich Plasma (PRP) injections to stimulate healing in my shoulder. Dr. Squires took the time to talk to me about the procedure, my concerns, and the expected outcome. I have had great success with the PRP injection and would highly recommend Dr. Squires.
