In the Regenerative Medicine and Orthobiologics field, there has for some time been controversy concerning certain aspects of Platelet Rich Plasma (PRP).
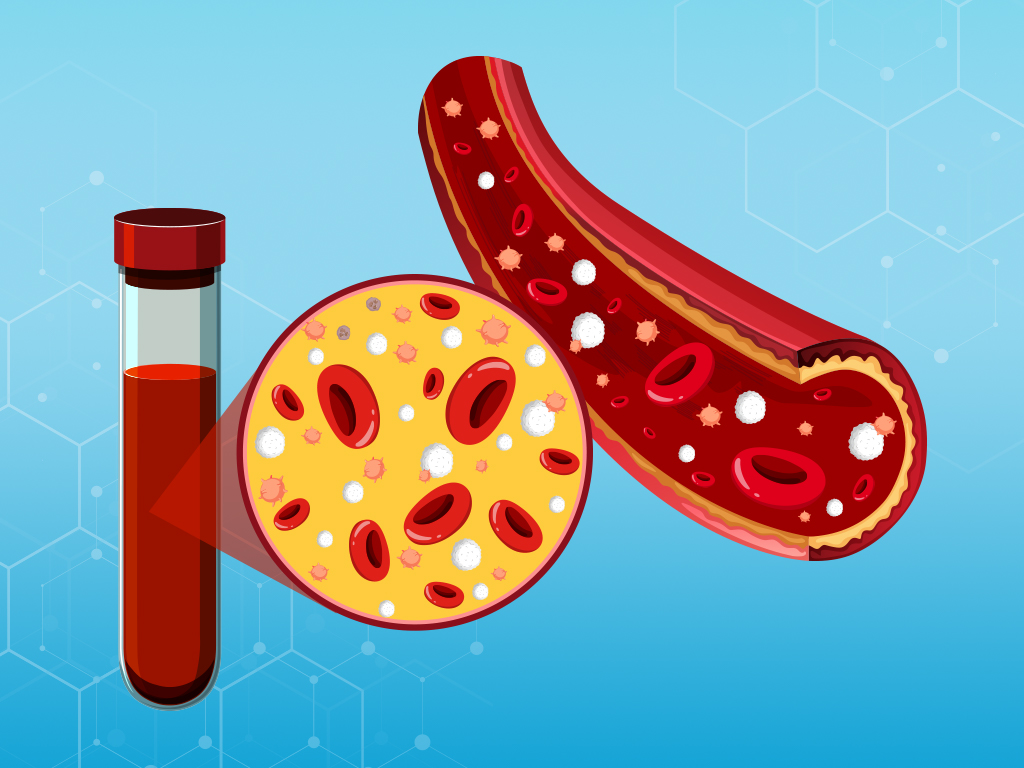
For those unfamiliar, Platelet Rich Plasma (PRP) involves using your own blood plasma and platelets as an enriched source of growth factors and immune cells to stimulate healing of bone and soft tissue.
This therapy can be utilized for minor tearing of ligaments and tendons, osteoarthritis, plantar fasciitis, ligament instability, and overuse injuries, as well as for aesthetic purposes. Learn more about how we use PRP here »
However, there are opinions (and in my mind misconceptions) that some components of PRP are bad – namely leukocytes.
There is a belief amongst many Regenerative Medicine doctors that a leukocyte poor (LP) PRP is more effective than a PRP product that contains leukocytes. Leukocytes are the white blood cells found in the blood.
There is a view that the only important component of PRP is the platelets that contain the growth factors.
This belief arose from concerns that leukocytes in leukocyte-rich PRP (LR-PRP) might exacerbate inflammation and contribute to further tissue pathology. And possibly that RBCs could leak compounds that may lead to oxidative damage in the treated tissue.
These concerns turned into accepted understanding even though they have no clinical evidence available to back them up.
When one researches deeper into the science of PRP, we find that there is a copious amount of literature to support the concept that all components of the blood are necessary to achieve an optimal result, including leukocytes.
But not every case is the same.
So now, let’s go into why these leucocytes/blood cells are important for healing.
Importance of White Blood Cells (WBCs):

- White blood cells (WBCs) are important effector cells of the innate immune system that cleanse a wound and prevent infection. WBCs also signal healing cascades that clear the wound of dead and damaged tissues and stimulate activation of growth factors that direct the conversion into vascularized and viable tissue.
- Appropriate signaling by WBCs allows immune cells to engage with their environment and increase the ability to generate and release an assortment of cytokines, growth factors, bioactive lipids, and proteases. These all contribute to helping modulate and direct the inflammatory response, reducing tissue damage as well as providing an environment for regeneration and repair.
Importance of Red Blood Cells (RBCs):
- RBCs accelerate and amplify thrombin generation. Thrombin is a powerful natural platelet activator that promotes an efficient inflammatory response and release of growth factors that can lead to wound repair.
- RBCs will stimulate immune cells such as phagocytes which release anti-inflammatory cytokines such as IL-10 and TGF-β1. This results in complete platelet activation. It’s also important for shifting the inflammatory response – limiting the magnitude and duration of platelet-driven inflammation.
Conclusion:
It is the synergistic relationship between platelets, RBCs and WBCs that is essential for an appropriate healing response leading to effective regeneration and repair of tissues.
The appropriate use of the right approach for the right outcome is also important. Meaning a good physician will adjust as needed to get the best outcome for each situation.
If you’d like to discuss using PRP therapies to help your pain and healing, schedule your initial consult today »
Reference:
- Arnoczky SP, Sheibani-Rad S. The basic science of platelet-rich plasma (PRP): what clinicians need to know. Sports Med Arthrosc Rev. 2013 Dec;21(4):180-5. doi: 10.1097/JSA.0b013e3182999712. Erratum in: Sports Med Arthrosc. 2014 Jun;22(2):150. Shebani-Rad, Shahin [corrected to Sheibani-Rad, Shahin]. PMID: 24212364.
- Boswell SG, Cole BJ, Sundman EA, Karas V, Fortier LA. Platelet-rich plasma: a milieu of bioactive factors. Arthroscopy. 2012 Mar;28(3):429-39. doi: 10.1016/j.arthro.2011.10.018. Epub 2012 Jan 28. PMID: 22284405.

